The Intersection between Liver Disease and the Microbiome
Published on: 20 Oct 2023
The Gut-liver axis.
The gut-liver axis refers to the bidirectional relationship between the gut microbiome and the liver. This relationship arises from the integration of signals produced by various factors such as diet, genetics, and the environment.
The portal vein connects the liver and the gastrointestinal tract and allows the transportation of gut-derived products through the blood to the liver. The liver then secretes bile and antibodies back into the gut – this feedback system is the gut-liver axis (1). Therefore, the gut microbiome plays an important role in the pathophysiology of many liver diseases. The liver is the organ that is in closest contact with the intestinal tract and is therefore exposed to a substantial number of bacterial components and metabolites (2).
Various liver diseases such as alcoholic liver disease (ALD) and non-alcoholic fatty liver disease (NAFLD) have been associated with an altered microbiome, known as dysbiosis. This dysbiosis can influence the degree of inflammation, fibrosis, and hepatic steatosis through interactions with the immune system and other cell types (2).
The gut microbiome consists of trillions of different microorganisms such as bacteria, viruses, and fungi, which live in the gastrointestinal tract. These microorganisms have a significant impact on the pathological and physiological processes of their host – there is a mutual relationship resulting in many different roles in the body such as maintaining a normal immune system, and nutrient digestion and absorption (3).
A major role of the gut microbiome in liver disease is supported by the accumulating evidence that several complications of liver disease such as hepatic encephalopathy can be efficiently treated by prebiotics, probiotics, and antibiotics (4). A better understanding of the gut microbiome and its role in liver diseases could provide a clearer picture of these complex disorders and provide the basis for novel therapies.
Non-alcoholic fatty liver disease.
NAFLD is a subtype of liver disease associated with obesity, type 2 diabetes mellitus (T2DM), insulin resistance, hypertension, and metabolic syndrome. Non-alcoholic steatohepatitis (NASH) is a subtype of NAFLD and can lead to liver fibrosis, cirrhosis, and hepatocellular carcinoma (HCC) (5). NAFLD is one of the most common types of chronic liver disease in the general population, and it is projected that the burden of end-stage liver disease because of NAFLD will triple by 2030. NAFLD is often associated with excess adiposity, and the microbiome in overweight individuals is less diverse than that in lean individuals (5).
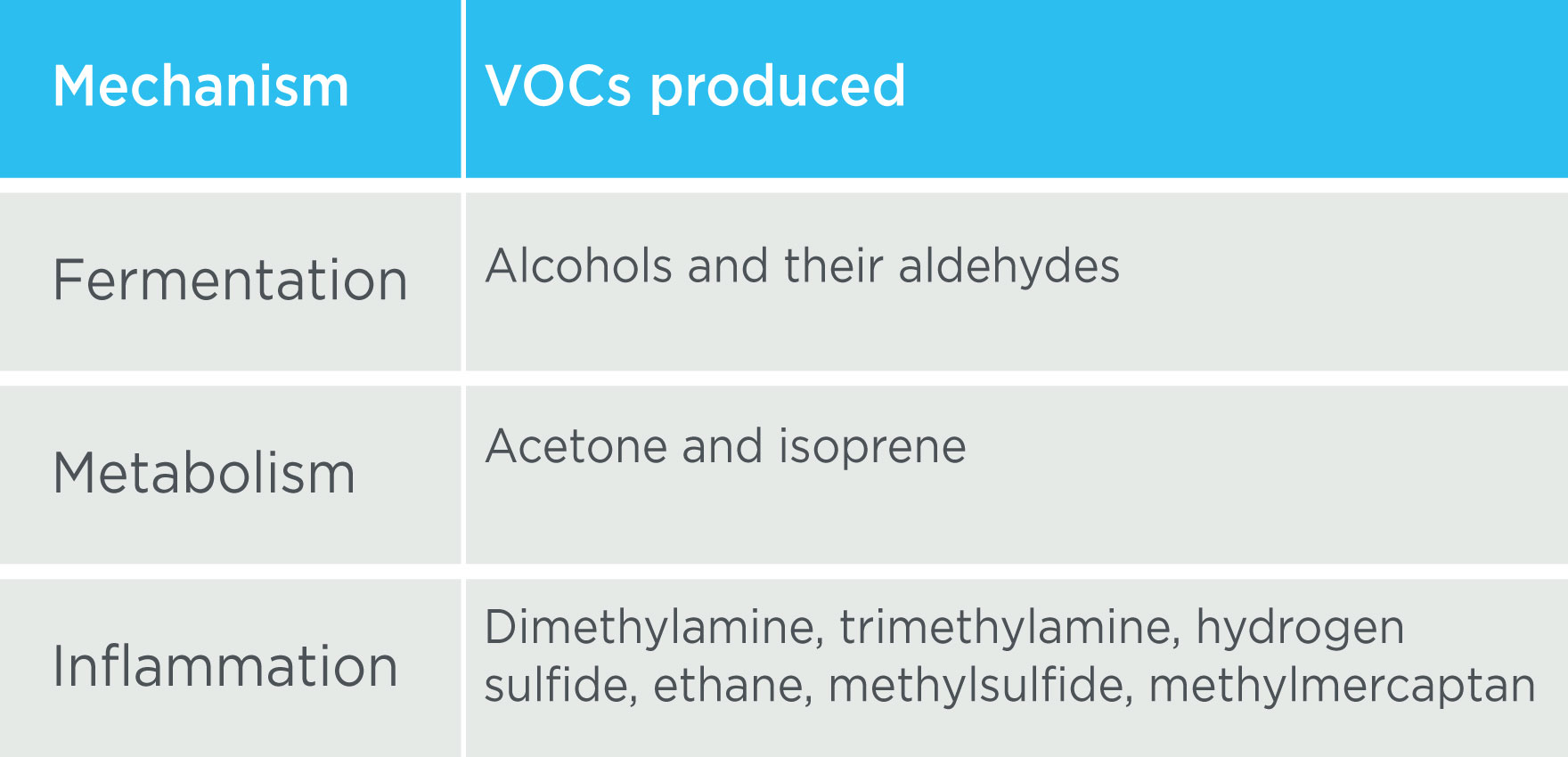
Research has found that patients with NASH have a lower proportion of Bacteroidetes (6) compared to healthy controls, and patients with NAFLD have a higher proportion of Escherichia, Anaerobacter, Lactobacillus and Clostridium compared to healthy controls (7). Products from these microbes such as endotoxins can get translocated in the portal circulation, resulting in cytokine activation and the release of interleukins which stimulate an inflammatory reaction, possibly leading to hepatic inflammation and fibrosis (3). There are multiple different volatile organic compounds (VOCs) that may be measured in breath from the mechanisms occurring in NAFLD (Table 1). Microbes can also produce ethanol, which can increase gram-negative bacterial growth and intestinal permeability, thereby promoting the uptake of inflammatory mediators.
Ethanol and liver disease.
The gut microbiome is thought to play many roles in the pathogenesis of non-alcoholic liver diseases. Higher levels of ethanol-producing bacteria are seen in patients with non-alcoholic steatohepatitis (NASH) such as Escherichia (9), and high levels of circulating microbial ethanol have been thought to result from functional impairment of hepatic insulin-dependent alcohol dehydrogenase (ADH). If produced chronically in relevant amounts, microbially produced ethanol could have the ability to alter lipid and glucose metabolism and induce steatosis and inflammation in the liver (10).
The liver has the capacity to metabolize ethanol via the ADH and cytochrome P450 pathways. This results in low circulating levels of ethanol in the blood of healthy individuals. However, in patients with liver disease, specifically end-stage liver disease, microbial ethanol production can exceed the liver’s capacity to remove ethanol from the portal circulation (10). The ethanol therefore remains in the blood and can then circulate throughout the body.
Ethanol is volatile and can be detected in breath.
Ethanol is a volatile compound which is readily detectable in exhaled breath. Ethanol produced in the gut can enter the bloodstream, which circulates throughout the body and can enter the air in the lungs via the network of blood vessels surrounding the alveolar membrane. This air is enriched for volatile compounds from throughout the body and is then exhaled. Therefore, ethanol in the breath can provide a window into the microbial metabolism ongoing in the gastrointestinal tract and could be used to investigate the presence of liver disease. Ethanol is one example of a volatile compound that can be linked to microbial activity associated with the liver, but there are hundreds of other biologically relevant VOCs present in breath.
As breath is a virtually inexhaustible resource, large volumes can be collected at frequent intervals, and compounds can also be pre-concentrated prior to analysis. This makes breath analysis capable of real-time longitudinal analysis of volatile metabolites, and ethanol can be a key biomarker for liver disease in clinical studies. There are many more volatile compounds in our VOC Atlas, a catalog of identified volatile organic compounds (VOCs) that are commonly found on breath, many of which have been associated with liver disease.
Our Breath Biopsy OMNI service provides everything you might need to start using breath analysis, including expert advice from our team of scientists. We are the world leaders in Breath Biopsy, and we are here to help you to include breath analysis in your research.
If you have any questions of would like more information, please do not hesitate to contact us to discuss investigating breath VOC biomarkers for liver disease, the microbiome, or other diseases of interest.
References.
- Albillos A, Gottardi A de, Rescigno M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J Hepatol. 2020 Mar 1;72(3):558–77. DOI: 10.1016/j.jhep.2019.10.003
- Tilg H, Cani PD, Mayer EA. Gut microbiome and liver diseases. Gut. 2016 Dec 1;65(12):2035–44. DOI: 10.1136/gutjnl-2016-312729
- Albhaisi SAM, Bajaj JS, Sanyal AJ. Role of gut microbiota in liver disease. Am J Physiol-Gastrointest Liver Physiol. 2020 Jan;318(1):G84–98. DOI: 10.1152/ajpgi.00118.2019
- Dalal R, McGee RG, Riordan SM, Webster AC. Probiotics for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017 Feb 23;2017(2):CD008716. DOI: 10.1002/14651858.CD008716.pub3
- Younossi ZM. Non-alcoholic fatty liver disease – A global public health perspective. J Hepatol. 2019 Mar 1;70(3):531–44. DOI: 10.1016/j.jhep.2018.10.033
- Mouzaki M, Comelli EM, Arendt BM, Bonengel J, Fung SK, Fischer SE, et al. Intestinal microbiota in patients with nonalcoholic fatty liver disease. Hepatology. 2013;58(1):120–7. DOI: 10.1002/hep.26319
- Jiang W, Wu N, Wang X, Chi Y, Zhang Y, Qiu X, et al. Dysbiosis gut microbiota associated with inflammation and impaired mucosal immune function in intestine of humans with non-alcoholic fatty liver disease. Sci Rep. 2015 Feb 3;5(1):8096. DOI: 10.1038/srep08096
- Solga SF. Breath volatile organic compounds for the gut-fatty liver axis: Promise, peril, and path forward. World J Gastroenterol WJG. 2014 Jul 21;20(27):9017–25. DOI: 10.3748/wjg.v20.i27.9017
- Zhu L, Baker SS, Gill C, Liu W, Alkhouri R, Baker RD, et al. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: A connection between endogenous alcohol and NASH. Hepatology. 2013;57(2):601–9. DOI: 10.1002/hep.26093
- Meijnikman AS, Davids M, Herrema H, Aydin O, Tremaroli V, Rios-Morales M, et al. Microbiome-derived ethanol in nonalcoholic fatty liver disease. Nat Med. 2022 Oct;28(10):2100–6. DOI: 10.1038/s41591-022-02016-6
Quick Start Guide: Everything you need to know about how breath analysis can be used in liver disease research