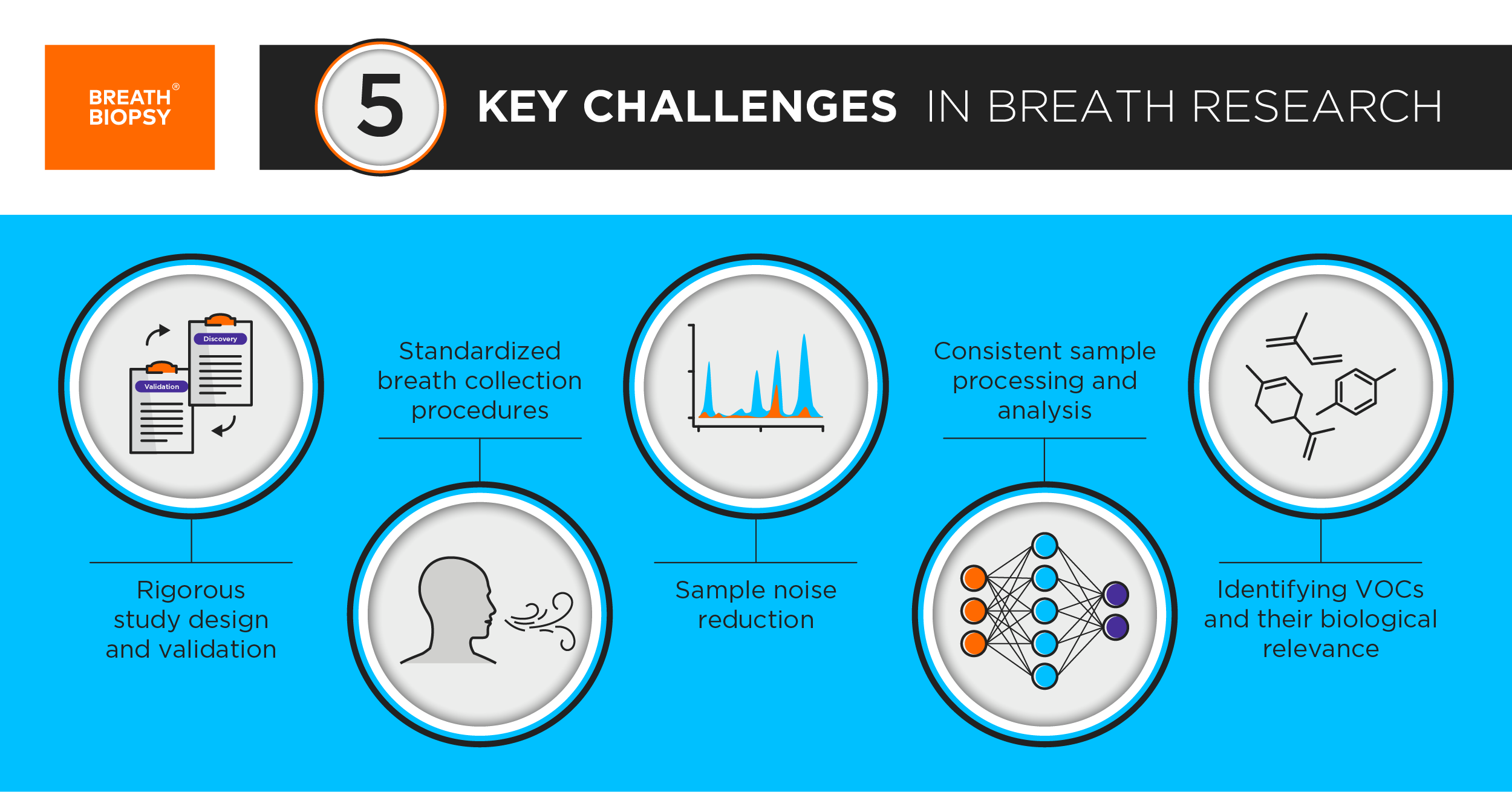
5 Key Challenges in Breath Research
Published on: 10 Sep 2019
The concept of using breath samples to identify changes linked with health and disease is not new. For decades researchers have been investigating the gas composition of breath as well as the volatile organic compounds (VOCs) in exhaled air to tell us more about our biology and health (Download our free ebook Breath Biopsy: The Complete Guide for details). In the genomics era, new technologies and an increased emphasis on high-throughput biological analysis and metabolomics have helped to expand the breath research field and interest in breathomics has grown rapidly [1].
Breath testing offers a straightforward, non-invasive way to monitor our biology, providing a potential tool for the early detection of diseases and optimization of treatment through precision medicine. Here we look at some of the methodological, biological and analytical challenges that are important to consider when designing breath studies to produce valuable, high-quality results.
Biomarkers for disease must be thoroughly validated before they can be used to diagnose illnesses and select treatments. This is essential for tests seeking regulatory approval from bodies like the FDA. To date, most studies in breath research have focused solely on biomarker discovery. As such, many breath biomarkers have been proposed for various diseases but few have been fully validated. Together, these studies demonstrate the wide-ranging potential of breath analysis but more studies now need to be designed directly with approval procedures and applications in mind.
Discovery studies have typically been small and collected samples from a single location. This creates issues with overfitting of data, where the small sample size is not suitably representative of the wider population. As a result, discrimination models based on the data perform poorly when applied to new datasets. In the ideal case, any prospective model should be validated using an independent cohort (e.g. Schleich et al. 2019 [2]). To date, few studies in the breath field have taken this approach. The Standards for the Reporting of Diagnostic Accuracy Studies (STARD) guidelines [3] and Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement [4] provide guidance for study design that encourage consideration of the need for quality validation at the earliest stages of study design. There is also a need to undertake a wider range of confirmatory studies based on the published results of other researchers.
To be truly representative, validation studies must seek to recruit subjects belonging to the intended use population not just a replicate of the discovery study. This ensures that a discrimination model can be usefully applied and meets the requirements for regulatory approval. Such populations and user settings usually introduce a greater deal of real life variability compared to the biomarker discovery set.
Rigorous validation can be strongly complemented by studying the biological origins of target VOC biomarkers to identify a clear association to relevant metabolic changes (see Challenge 5). Longitudinal studies and repeated sampling of subjects can also help to assess the robustness of biomarker signals relative to a changing background. Similarly, meta-analyses (like the recent one examining breath biomarkers of tuberculosis [5]) can identify and highlight themes across existing independent investigations.
VOC biomarkers typically occur in low abundance in exhaled breath so reliable collection and accurate detection are key to identifying suitable biomarkers. As with any emerging technology, a plethora of breath collection techniques have been developed by different researchers. Before breath testing can succeed in the clinic, we need to move towards a standardized methodology that produces consistent and reproducible results independent of context and without the need for specialist skills or equipment.
Both the type of breath and the volume collected vary greatly between studies and the act of collecting a breath sample can affect the results [6, 7]. Studies have also collected breath in everything from 20ml bottles [8] to 5 litre bags [9]. Both the European Respiratory Society Task Force [10] and the Breathe Free Project have worked to better standardize breath collection to ensure comparable results across studies. Through Breathe Free, we collaborated with leaders in breath research to develop the ReCIVA® Breath Sampler to improve standardization in breath collection.
By pre-concentrating samples on adsorbent tubes ReCIVA can collect more VOCs from a larger volume of air, offering the potential for greater sensitivity [9]. The pre-concentrated samples remain stable for longer at room temperature and are smaller, easier to transport and easier to store. In addition, measuring the volume of breath collected, collecting specific breath fractions (see Challenge 3) and collecting samples in a stable form have benefits for processing and analysis of samples.
Increasing sensitivity to detect low abundance VOC also increases the need for effective noise reduction in breath collection and analysis. Breath samples contain both exogenous and endogenous VOCs. Exogenous VOCs can derive from environmental (air pollution, cleaning products) and dietary (food, drink) sources and are a large component of VOCs in exhaled breath. While endogenous VOCs can be either local (arising from the airways, stomach or microbiome) or systemic (transferred into breath from the blood) [11, 12].
Reducing noise in samples depends largely on what VOCs a particular study is designed to investigate. Exogenous VOCs are often in higher abundance so can be easier to detect [13]. For more on how exogenous VOCs can be used in breath testing, visit our EVOC® Probes page. By contrast, many studies focus on endogenous VOCs and in these studies it is beneficial to exclude other sources of VOCs as much as possible. As such, steps can be taken to minimising exogenous VOC levels in breath samples to improve the detection of relevant breath biomarkers.
Controlling test subject behaviours, discouraging eating, drinking, smoking etc. for a period of time before breath collection is a widely used approach. This can be useful but is best applied in moderation, as excessive restrictions could limit future application of breath tests in the clinic.
Tools like the CASPER™ Portable Air Supply can significantly reduce environmental VOCs in breath samples. This can be particularly beneficial in multi-site studies since exogenous VOC profiles are affected by geographical location [14]. The ReCIVA Breath Sampler is also able to collect specific breath fractions, reducing noise from internal VOC sources such as the mouth, upper airways and/or stomach. Once breath biomarkers have been identified and validated for specific conditions, the need for background reduction may become less important as, in many cases, more targeted chemical analyses can be used, making it easier to identify key VOC profiles despite background noise.
GC-MS is widely accepted as the gold standard for chemical analysis of breath samples for VOC biomarker discovery [15, 16]. However, it requires sophisticated, expensive equipment and specialized training, limiting its usefulness in a clinical setting. In addition, biomarker discovery based purely upon GC-MS patterns must overcome issues with instrument calibration, unknown biases and the need for biological validation (see Challenge 5) Alternatives that show promise for targeted analyses of validated biomarkers in the clinic include eNose sensors and FAIMS technologies, like those developed by Owlstone. Such approaches are best applied in validation studies to detect known target biomarkers.
Beyond chemical analysis, an even greater range of computational approaches – support vector machines, regression analysis, random forest, neural networks etc. – are being applied to generate discriminatory tests from breath samples (see Challenge 1 for the importance of sample size in statistical analysis).
The number of different approaches and the lack of standardization clearly limit the ability to compare and combine datasets [17]. As work continues to identify breath biomarkers in different contexts, it’s important to continue exploring methods of biomarker research and identification to ensure we produce the most robust and reliable results that can also be practically implemented for diagnostic uses. By being clear about our methodologies and seeking to understand how different results compare we can seek to improve comparability across studies.
As mentioned in Challenge 1, there is a need to understand the chemical identity and biological origins of VOCs in breath. Current discovery studies identify compounds as molecular features in GC-MS spectra but it’s not always possible to link these to specific chemical structures [18, 19]. VOCs are often poorly represented in libraries of standard mass spectra, so identification is not straightforward. We must continue to identify and catalogue VOC spectra from GC-MS and other relevant analysis methods so that more VOCs in breath can be chemically identified. We must also use caution in assuming that tentative IDs from libraries are always correct, and include more standards and biological characterization in our studies.
Even once the chemical identity of a VOC is known, few VOCs have been conclusively linked to biological processes and more research is needed to identify the biological origins of VOCs, particularly in relation to specific diseases. The need to understand these causal relationships has been explored in depth by Rianne Fijten in her blog post, but knowing where biomarkers come from helps to validate their relevance and provides new insights into the mechanisms and effects of different diseases.
Breath analysis has great potential to improve human health while reducing strain on healthcare systems by providing easy to access screening for a wide range of health conditions. Technology has advanced to a stage where this goal is becoming attainable and the remaining challenges focus on the need for greater planning, standardization and coordination in how we approach the identification and validation of breath biomarkers. By addressing these challenges we can move the breath analysis field forward and begin to realise the clinical potential of this powerful detection approach.
The key challenges in breath research are discussed further in this review [20].
Download Breath Biopsy: The Complete Guide to explore the many possible applications of breath research and how Breath Biopsy is supporting progress in this fast growing field.
References
- www.ersnet.org/the-society/news/ers-task-force-develops-technical-standard-on-exhaled-biomarkers-in-lung-disease
- Schleich et al. (2019) Exhaled Volatile Organic Compounds Are Able to Discriminate between Neutrophilic and Eosinophilic Asthma, Am J Respir Crit Care Med, DOI: 10.1164/rccm.201811-2210OC
- www.stard-statement.org
- www.spirit-statement.org
- Saktiawatia et al. (2019) Diagnosis of tuberculosis through breath test: A systematic review, EBioMedicine, DOI: 10.1016/j.ebiom.2019.07.056
- Bikov et al. (2013) Standardised exhaled breath collection for the measurement of exhaled volatile organic compounds by proton transfer reaction mass spectrometry, BMC Pulmonary Medicine, DOI: 10.1186/1471-2466-13-43
- Dragonieri et al. (2007) An electronic nose in the discrimination of patients with asthma and controls., J Allergy Clin Immunol., DOI: 10.1016/j.jaci.2007.05.043
- Netzer et al. (2009) A new ensemble-based algorithm for identifying breath gas marker candidates in liver disease using ion molecule reaction mass spectrometry. Bioinformatics, DOI: 10.1093/bioinformatics/btp093
- https://www.owlstonemedical.com/media/uploads/files/Reciva_sorbentvsTedlar.pdf
- Horváth et al. (2017) A European Respiratory Society technical standard: exhaled biomarkers in lung disease., Eur Respir J, 10.1183/13993003.00965-2016
- Lourenço et al. (2014) Breath Analysis in Disease Diagnosis: Methodological Considerations and Applications, Metabolites, DOI: 10.3390/metabo4020465
- Leopold et al. (2019) Volatile organic compound profiles in outlet air from extracorporeal life-support devices differ from breath profiles in critically ill patients, ERJ Open Research, DOI: 10.1183/23120541.00134-2018
- Pleil et al. (2013) Clinical breath analysis: discriminating between human endogenous compounds and exogenous (environmental) chemical confounders., J Breath Res, DOI: 10.1088/1752-7155/7/1/017107
- Anal et al. (2013) Geographical variation in the exhaled volatile organic compounds, J Breath Res, DOI: 10.1088/1752-7155/7/4/047102
- Wang et al. (2018) Stability control for breath analysis using GC-MS, J Chromatog B., DOI: 10.1016/j.jchromb.2018.08.024
- Miekisch and Schubert (2006) From highly sophisticated analytical techniques to life-saving diagnostics: Technical developments in breath analysis, TrAC Trends in Analytical Chemistry, DOI: 10.1016/j.trac.2006.05.006
- Herbig and Beauchamp (2014) Towards standardization in the analysis of breath gas volatiles, J Breath Res, DOI: 10.1088/1752-7155/8/3/037101
- Zhang and Li (2010) A review of advances and new developments in the analysis of biological volatile organic compounds, Microchemical J, DOI: 10.1016/j.microc.2009.12.017
- Chin et al. (2018) Cross-platform mass spectrometry annotation in breathomics of oesophageal-gastric cancer, Scientific Reports, DOI: 10.1038/s41598-018-22890-w
- Boots et al. (2015) Exhaled Molecular Fingerprinting in Diagnosis and Monitoring: Validating Volatile Promises., Trends Mol. Med., DOI: 10.1016/j.molmed.2015.08.001
Download the Breath Biopsy Guide to learn about breath biomarkers and their applications