Breath VOC biomarkers for Asthma: where are we at in 2024?
We have combined our internal data with VOCs identified across the literature to present the most promising VOC biomarkers for asthma that could be translated into breath tests in the future.
| Disease Area: Respiratory, Asthma
Application: Biomarker Development Sample medium: Breath Analysis approach: Various (GC, GC-MS, TD-GC-MS, GCxGC-MS, GC-ToF-MS, GCxGC-ToF-MS, TD-GC-ToF-MS, NTD-GC-MS, GCxGC-HRToFMS, SIFT-MS, TD-GM/q-MS). Summary:
|
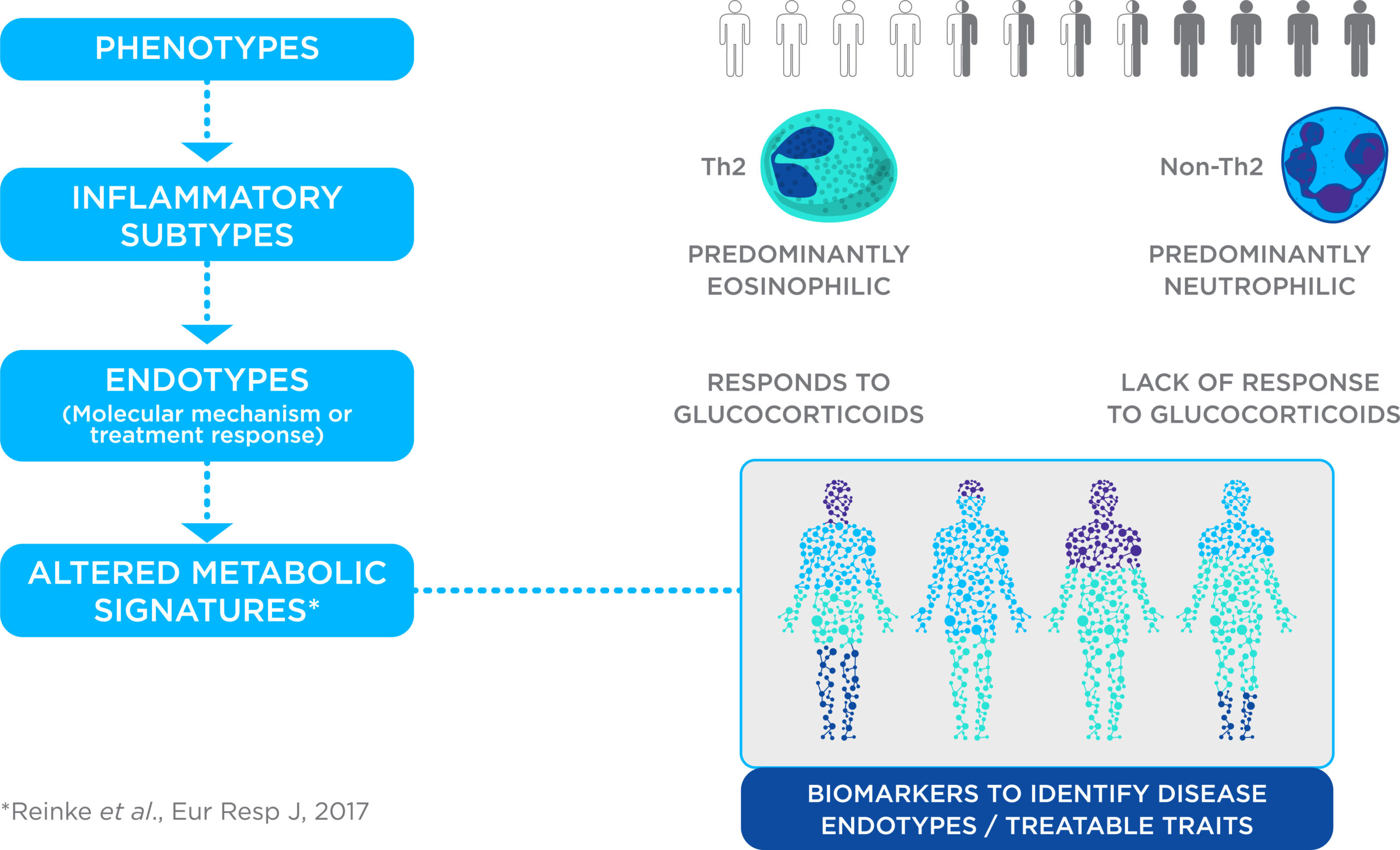
Asthma is a chronic inflammatory condition affecting millions of people worldwide, including approximately 12% of children aged 6 – 7 (1). Although all asthma patients experience a common set of symptoms (shortness of breath, chest tightness, wheezing when exhaling, etc.), the underlying disease mechanisms vary between patients, and this means that treatment selection is highly individual. A key distinction between asthma cases is the type of immune cells causing inflammation: eosinophilic or neutrophilic. Cases that are primarily eosinophilic typically respond well to glucocorticoid steroid treatments, whereas cases dominated by neutrophils show a poor response to steroids. Currently, the diagnosis of asthma is based on clinical history, physical examination, and lung function. However, the current diagnostic methods do not allow asthma to be diagnosed directly or to differentiate between phenotypes, therefore treatments are often prescribed via ‘trial and error’ approach. During this time, inappropriate treatments are prescribed resulting in unnecessary spending for healthcare systems, and periods of poor disease control with an increased risk of exacerbations for the patient.
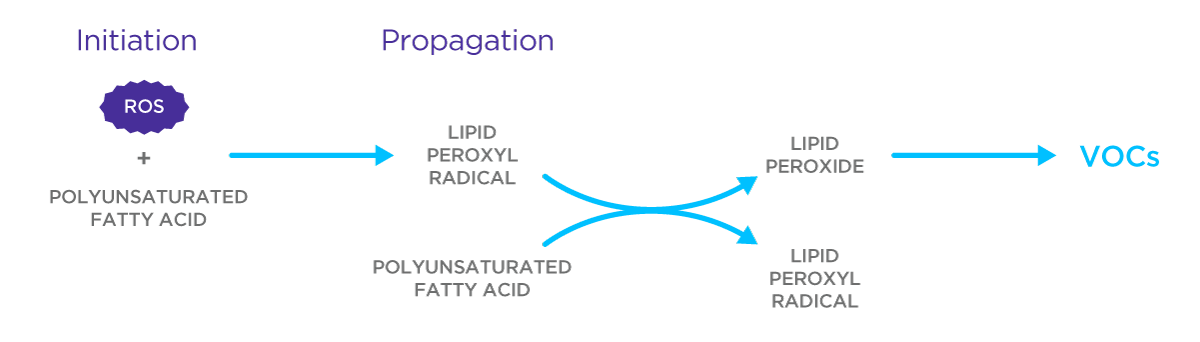
Breath contains hundreds of volatile organic compounds (VOCs), many of which are produced locally in the respiratory tract due to processes such as lipid peroxidation, that could serve as new biomarkers for asthma. VOCs can be produced by the immunological mechanisms that underpin asthma pathophysiology, and therefore potentially could be used as better biomarkers to stratify patients without the need for trial and error.
Asthma is one of the most studied respiratory diseases in terms of the VOCs in breath, likely due to both the importance of asthma as a common chronic respiratory condition with a significant impact on quality of life, and the potential clinical benefits that breath tests could provide. There is currently one breath test used in asthma diagnosis: Fractional Exhaled Nitric Oxide (FeNO), which is usually only used to support a diagnosis of asthma rather than as a conclusive biomarker, as there are cases of asthma (especially eosinophilic asthma) where FeNO may be low (2,3). Therefore, understanding how other informative volatiles in breath change in abundance in asthma could lead to the development of further diagnostic tests, that impart more detailed information about specific asthma phenotypes and underlying physiology in the respiratory tract.
Given the significant variability of volatile compounds among the human population, studies employing untargeted approaches without adequate controls can easily produce false positive hits when it comes to identifying candidate biomarkers. Therefore, it is important to cross-validate the findings of VOC composition associated with asthma across the literature and qualify which studies reported compounds that are highly likely to be genuine signals related to asthma pathophysiology, as opposed to background spurious signals. To this end, we completed a literature review combined with our internal data and will summarize the most promising VOC biomarkers for asthma (covering a broad range of studies across different asthma severities, age groups, and phenotypes in the first incidence) in this case study.
As of 6th March 2024 this combination of compounds from the literature and those arising from our internal data resulted in almost 200 unique VOCs that have been associated with asthma (4–26), which can be sorted into useful categories. The first is the group of asthma-associated VOCs that are in our Breath Biopsy VOC Atlas as “on-breath” (group 1), and the second are VOCs that are in our VOC Atlas but not routinely seen in healthy participants (group 2). Our VOC Atlas contains VOCs that have been carefully quantified for their presence in the breath (“on-breath”) in a population of heterogenous volunteers without any specific pathophysiologies, as opposed to originating from environmental contaminants, and all of the VOCs have undergone rigorous validation against standard references to confirm their identities. This means that the on-breath compounds could be associated with normal, healthy variation in the population, whereas group 2 compounds in the VOC Atlas are compounds that were not observed in individuals that could be considered to be healthy. This means that they may only be detectable in the breath of those with asthma and not in the breath of a healthy person – and so are promising to investigate further as potential breath VOC biomarkers of asthma. You can register for access to the Atlas here.
Of the approximately 200 compounds, 87 were contained with the VOC Atlas, of which 86% of the VOCs were identified in more than one paper as being associated with asthma. As most of the identified compounds that were not in the VOC Atlas were only mentioned in a single paper across the literature, the VOC Atlas may contain the key compounds that are more confidently able to be separated from spuriously significant compounds. Of the combined dataset of VOCs there were a total of 35 group 1 compounds, and 52 group 2 compounds that were altered in the breath of asthma patients. The chemical classes of the compounds that increased in asthmatic patients that were also group 2 are likely to give a clue as to the biological mechanism that produces them. Compared to group 1 compounds, there were 31% more alkanes, 10% more aldehydes, 10% more cyclic hydrocarbons group 2 compounds. This strongly suggests that lipid peroxidation is a major source of the altered volatile signature of the breath of asthmatic patients. Chronic inflammation is a key characteristic of asthma, a state which generates oxidative stress in the tissues of the respiratory tract. This results in the generation reactive oxygen species that can react with unsaturated fatty acids in the cell, and the subsequent release of characteristic volatile compounds like alkanes (27). Although lipid peroxidation has been associated with many inflammatory diseases, the different lipid compositions and redox enzyme complements of different cell types can result in a unique set of VOC lipid peroxidation products. In asthma, the inflammatory process occurs due to interactions between leukocytes, epithelial and stromal cells of the respiratory tract, and so could produce a unique pattern of volatiles in the breath (28).
These group 2 compounds are therefore strong candidate biomarkers to study further to investigate the asthma-related pathophysiology that leads to their changing of abundance in the breath. Also, normally on-breath compounds that decrease to the point of being indistinguishable from background signal in patients with asthma are strong candidate biomarkers to investigate further. To progress these biomarkers towards validation, and eventually translation into further breath tests for asthma in clinical use, more work needs to be done to link the characteristic changing levels of these compounds in the breath in asthma, and the underlying mechanisms responsible.
We can incorporate use of the Breath Biopsy VOC Atlas in your breath research as part of our Breath Biopsy OMNI® service to enhance and fast-track breath biomarker identification and validation. To find out more information about breath biomarkers for asthma, and other potential research studied involving the use of VOCs, please do not hesitate to contact us.
References
1. Prevalence | Background information | Asthma | CKS | NICE [Internet]. [cited 2023 Aug 16]. Available from: https://cks.nice.org.uk/topics/asthma/background-information/prevalence/
2. Stuehr DJ. Mammalian nitric oxide synthases. Biochim Biophys Acta. 1999 May 5;1411(2–3):217–30.
3. Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An Official ATS Clinical Practice Guideline: Interpretation of Exhaled Nitric Oxide Levels (FeNO) for Clinical Applications. Am J Respir Crit Care Med. 2011 Sep 1;184(5):602–15.
4. Alahmadi FH, Wilkinson M, Keevil B, Niven R, Fowler SJ. Short- and medium-term effect of inhaled corticosteroids on exhaled breath biomarkers in severe asthma. J Breath Res. 2022 Jul;16(4):047101.
5. Brinkman P, van de Pol MA, Gerritsen MG, Bos LD, Dekker T, Smids BS, et al. Exhaled breath profiles in the monitoring of loss of control and clinical recovery in asthma. Clin Exp Allergy. 2017 Sep;47(9):1159–69.
6. Brinkman P, Ahmed WM, Gómez C, Knobel HH, Weda H, Vink TJ, et al. Exhaled volatile organic compounds as markers for medication use in asthma. Eur Respir J. 2020 Feb;55(2):1900544.
7. Dragonieri S, Schot R, Mertens BJA, Le Cessie S, Gauw SA, Spanevello A, et al. An electronic nose in the discrimination of patients with asthma and controls. J Allergy Clin Immunol. 2007 Oct;120(4):856–62.
8. Gahleitner F, Guallar-Hoyas C, Beardsmore CS, Pandya HC, Thomas CP. Metabolomics pilot study to identify volatile organic compound markers of childhood asthma in exhaled breath. Bioanalysis. 2013 Sep;5(18):2239–47.
9. Ibrahim W, Wilde MJ, Cordell RL, Richardson M, Salman D, Free RC, et al. Visualization of exhaled breath metabolites reveals distinct diagnostic signatures for acute cardiorespiratory breathlessness. Science Translational Medicine. 2022 Nov 16;14(671):eabl5849.
10. Ibrahim B, Basanta M, Cadden P, Singh D, Douce D, Woodcock A, et al. Non-invasive phenotyping using exhaled volatile organic compounds in asthma. Thorax. 2011 Sep;66(9):804–9.
11. Klaassen EMM, van de Kant KDG, Jöbsis Q, van Schayck OCP, Smolinska A, Dallinga JW, et al. Exhaled biomarkers and gene expression at preschool age improve asthma prediction at 6 years of age. Am J Respir Crit Care Med. 2015 Jan 15;191(2):201–7.
12. Awano S, Takata Y, Soh I, Yoshida A, Hamasaki T, Sonoki K, et al. Correlations between health status and OralChromaTM-determined volatile sulfide levels in mouth air of the elderly. J Breath Res. 2011 Sep;5(4):046007.
13. Caldeira M, Barros AS, Bilelo MJ, Parada A, Câmara JS, Rocha SM. Profiling allergic asthma volatile metabolic patterns using a headspace-solid phase microextraction/gas chromatography based methodology. Journal of Chromatography A. 2011 Jun 17;1218(24):3771–80.
14. Caldeira M, Perestrelo R, Barros AS, Bilelo MJ, Morête A, Câmara JS, et al. Allergic asthma exhaled breath metabolome: a challenge for comprehensive two-dimensional gas chromatography. J Chromatogr A. 2012 Sep 7;1254:87–97.
15. Dallinga JW, Robroeks CMHHT, van Berkel JJBN, Moonen EJC, Godschalk RWL, Jöbsis Q, et al. Volatile organic compounds in exhaled breath as a diagnostic tool for asthma in children. Clin Exp Allergy. 2010 Jan;40(1):68–76.
16. Meyer N, Dallinga JW, Nuss SJ, Moonen EJC, van Berkel JJBN, Akdis C, et al. Defining adult asthma endotypes by clinical features and patterns of volatile organic compounds in exhaled air. Respir Res. 2014 Nov 28;15(1):136.
17. Monedeiro F, Monedeiro-Milanowski M, Ratiu IA, Brożek B, Ligor T, Buszewski B. Needle Trap Device-GC-MS for Characterization of Lung Diseases Based on Breath VOC Profiles. Molecules. 2021 Jan;26(6):1789.
18. Paredi P, Kharitonov SA, Barnes PJ. Elevation of Exhaled Ethane Concentration in Asthma. Am J Respir Crit Care Med. 2000 Oct;162(4):1450–4.
19. Robroeks CM, Berkel JJ van, Jöbsis Q, Schooten FJ van, Dallinga JW, Wouters EF, et al. Exhaled volatile organic compounds predict exacerbations of childhood asthma in a 1-year prospective study. European Respiratory Journal. 2013 Jul 1;42(1):98–106.
20. Schleich FN, Zanella D, Stefanuto PH, Bessonov K, Smolinska A, Dallinga JW, et al. Exhaled Volatile Organic Compounds Are Able to Discriminate between Neutrophilic and Eosinophilic Asthma. Am J Respir Crit Care Med. 2019 Aug 15;200(4):444–53.
21. Sharma R, Zang W, Zhou M, Schafer N, Begley LA, Huang YJ, et al. Real Time Breath Analysis Using Portable Gas Chromatography for Adult Asthma Phenotypes. Metabolites. 2021 May;11(5):265.
22. Smolinska A, Klaassen EMM, Dallinga JW, Kant KDG van de, Jobsis Q, Moonen EJC, et al. Profiling of Volatile Organic Compounds in Exhaled Breath As a Strategy to Find Early Predictive Signatures of Asthma in Children. PLOS ONE. 2014 Apr 21;9(4):e95668.
23. Sola-Martínez RA, Lozano-Terol G, Gallego-Jara J, Morales E, Cantero-Cano E, Sanchez-Solis M, et al. Exhaled volatilome analysis as a useful tool to discriminate asthma with other coexisting atopic diseases in women of childbearing age. Sci Rep. 2021 Jul 5;11(1):13823.
24. Vliet DV, Smolinska A, Jöbsis Q, Rosias PPR, Muris JWM, Dallinga JW, et al. Association between exhaled inflammatory markers and asthma control in children. J Breath Res. 2016 Feb;10(1):016014.
25. Vliet D van, Smolinska A, Jöbsis Q, Rosias P, Muris J, Dallinga J, et al. Can exhaled volatile organic compounds predict asthma exacerbations in children? J Breath Res. 2017 Mar;11(1):016016.
26. Shahrokny P, Maison N, Riemann L, Ehrmann M, DeLuca D, Schuchardt S, et al. Increased breath naphthalene in children with asthma and wheeze of the All Age Asthma Cohort (ALLIANCE). J Breath Res. 2023 Oct 12;18(1).
27. Ratcliffe N, Wieczorek T, Drabińska N, Gould O, Osborne A, Costello BDL. A mechanistic study and review of volatile products from peroxidation of unsaturated fatty acids: an aid to understanding the origins of volatile organic compounds from the human body. J Breath Res. 2020 May;14(3):034001.
28. Rahman I, Kelly F. Biomarkers in breath condensate: a promising new non-invasive technique in free radical research. Free Radic Res. 2003 Dec;37(12):1253–66.