Can Breath VOCs Reflect Changes to the Microbiome?
Published on: 22 Sep 2024
Introduction
The human body is composed of around 30 trillion cells, and is home to roughly 40 trillion bacteria, 95% of which are found in the gut comprising the gut microbiome (1,2). From regulating our immune system to influencing the development of major diseases, scientists are rapidly uncovering the significant influence of these microbes on our health and disease (3). In particular, the imbalance of the gut microbiome composition, or dysbiosis, is well characterized to be associated with diseases such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) (3). Certain interventions like probiotics and antibiotics can alter the gut microbiome and have the potential to treat diseases impacted by dysbiosis. Therefore, being able to monitor the response of the gut microbiome to these interventions is important in understanding their effects.
Dr Andrew Kau from the Washington University School of Medicine recently presented at the Breath Biopsy Conference 2024 on ‘The Breath Volatilome is Shaped by the Gut Microbiota’. You can watch Dr. Kau’s talk, as well as the other presentations from the conference here.
Monitoring the microbiome using VOCs
There are many ways to monitor the gut microbiome, with DNA analysis of fecal samples being the most commonly used. Alternatively, blood sampling can be used as small-molecule microbiome metabolites can enter the bloodstream from the gut.
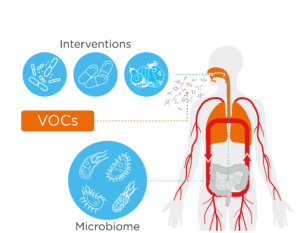
A growing amount of research has begun supporting the analysis of volatile organic compounds (VOCs). VOCs are carbon-based compounds that are gaseous at room temperature and can originate from metabolic byproducts, including those from the microbiome, with evidence supporting their use as biomarkers in gastrointestinal diseases (7,8). Breath VOCs are of particular interest due to their non-invasive nature, improving patient comfort and in turn patient recruitment to clinical trials. These VOCs can originate from the gut microbiome, enter the bloodstream, and escape into the air in the lungs to be subsequently exhaled. They can be collected at home to support decentralized clinical trial designs, and they allow for real-time analysis of microbial metabolism in the gut (8).
These monitoring techniques have enabled the understanding of how the microbiome can respond to interventions that alter it.
Interventions can alter the microbiome, which can be detected using breath VOCs
Dysbiosis can be caused by oral antibiotics killing beneficial gut bacteria in addition to the intended bacterial target (9). A prime example of antibiotic-induced dysbiosis is a Clostridium difficile (C.diff) infection. C.diff is normally found in the gut and kept at bay by other gut bacteria. However, when these bacteria are killed by antibiotic exposure, C.diff can multiply and produce toxins leading to diarrhea and even death (9,10). Studies have also shown associations between antibiotic usage altering the microbiome, and the development of obesity and type 1 diabetes (9). An interesting case report followed the effects of antibiotics on the gut microbiome in an individual. Fecal DNA analysis found that many residential gut bacteria were altered following antibiotic treatment, especially in members of the Bacteroides genus. At the same time, many breath VOCs were altered (11). Similarly, a study by Van Malderen et al. showed that VOCs could differentiate IBS patients based on whether they were undergoing antibiotic treatment or not. Notably, these differences were identified with similar accuracy using breath and fecal VOCs
On the other hand, probiotics like yogurt contain live bacteria that can introduce beneficial bacteria and help restore the gut microbiome balance in those with conditions linked to dysbiosis (12). Studies have supported probiotic use for the prevention of atopic dermatitis, ulcerative colitis, IBS, and even C.diff infections (13,14). The same study by Van Malderen et al. previously discussed was able to differentiate IBS patients based on probiotic usage using breath and fecal VOCs with similar accuracy (8). Again, this highlights the ability of breath VOCs to reflect changes in microbial composition. Prebiotics are thought to support the gut microbiome in a similar way but differ from probiotics as they are considered food for gut bacteria, typically referring to high-fiber foods. A study showed that the levels of 13 breath VOC were altered following the prebiotics (fiber) intake, as compared to a placebo, with sequencing revealing that the Mitsuokella genus could have been responsible for some of the changes (15). A follow-up study utilizing dietary fiber further identified correlations between bacterial species and breath VOCs, including faecalibacterium with butyric acid, and ruminococcaceae and lachnospiraceae with propionic acid (16). These studies show that prebiotic interventions can modify metabolite production by the gut microbiome, and these changes are correlated with changes in exhaled breath VOCs.
Other factors can also have unintended effects on our gut health, which can be revealed via breath VOC analysis. For example, breath VOC analysis discovered that iron supplementation resulted in an increase in short-chain fatty acids, a finding linked to increased gut health (17). The same study also revealed a decrease in hydrogen sulphide following iron supplementation.
These studies are among the several that have shown the potential of breath VOCs as a powerful tool to support research investigating changes in the microbiome following interventions. Other breath gases such as hydrogen and methane are clinically validated biomarkers for gut microbiome activity and are currently used in-clinic to diagnose conditions such as small intestinal bacterial overgrowth (SIBO) and carbohydrate malabsorption conditions. New technologies such as the OMED Health Breath Analyzer can measure hydrogen and methane in exhaled breath to help monitor the gut microbiome at home, and can support studies looking to investigate the effect of interventions on the microbiome through longitudinal, repeat sampling.
Conclusion
In conclusion, many factors can have profound effects on our gut microbiome, which in turn, can significantly affect our health. It is therefore worthwhile to develop technologies that can study the response of our gut to such interventions. Currently, fecal analysis of DNA and end-product metabolites is popular, but the analysis of breath VOCs and gases is emerging as a less invasive and more practical alternative that can support longitudinal and real-time monitoring.
If you are interested in seeing how breath analysis could be incorporated into your research, please do not hesitate to contact us.
References
- Sender R, Fuchs S, Milo R. Revised Estimates for the Number of Human and Bacteria Cells in the Body. PLoS Biol. 2016 Aug 19;14(8):e1002533. doi: 10.1371/journal.pbio.1002533
- Dupont HL, Jiang ZD, Dupont AW, Utay NS. The Intestinal Microbiome In Human Health And Disease. Trans Am Clin Climatol Assoc. 2020;131:178–97. PMCID: PMC7358474
- Afzaal M, Saeed F, Shah YA, Hussain M, Rabail R, Socol CT, et al. Human gut microbiota in health and disease: Unveiling the relationship. Front Microbiol. 2022;13:999001. doi: 10.3389/fmicb.2022.999001
- Thomas V, Clark J, Doré J. Fecal microbiota analysis: an overview of sample collection methods and sequencing strategies. Future Microbiol. 2015;10(9):1485–504. doi: 10.2217/fmb.15.87
- Li X meng, Shi X, Yao Y, Shen Y cun, Wu X ling, Cai T, et al. Effects of Stool Sample Preservation Methods on Gut Microbiota Biodiversity: New Original Data and Systematic Review with Meta-Analysis. Microbiol Spectr. 11(3):e04297-22. doi: 10.1128/spectrum.04297-22
- Lee YY, Erdogan A, Rao SSC. How to Assess Regional and Whole Gut Transit Time With Wireless Motility Capsule. J Neurogastroenterol Motil. 2014 Apr;20(2):265–70. doi: 10.5056/jnm.2014.20.2.265
- Hosfield BD, Pecoraro AR, Baxter NT, Hawkins TB, Markel TA. The Assessment of Fecal Volatile Organic Compounds in Healthy Infants: Electronic Nose Device Predicts Patient Demographics and Microbial Enterotype. J Surg Res. 2020 Oct;254:340–7. doi: 10.1016/j.jss.2020.05.010
- Van Malderen K, Hanning N, Lambrechts H, Haverhals T, Van Marcke S, Ceuleers H, et al. Volatile organic compound profiling as a potential biomarker in irritable bowel syndrome: A feasibility study. Front Med. 2022 Aug 4;9:960000. doi: 10.3389/fmed.2022.960000
- Patangia DV, Anthony Ryan C, Dempsey E, Paul Ross R, Stanton C. Impact of antibiotics on the human microbiome and consequences for host health. MicrobiologyOpen. 2022 Jan 13;11(1):e1260. doi: 10.1002/mbo3.1260
- Clostridium difficile [Internet]. NHS inform. [cited 2024 Aug 7]. Available from: https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/clostridium-difficile/
- Shahi F, Forrester S, Redeker K, Chong JPJ, Barlow G. Case Report: The effect of intravenous and oral antibiotics on the gut microbiome and breath volatile organic compounds over one year. Wellcome Open Res. 2022 Dec 5;7:50. doi: 10.12688/wellcomeopenres.17450.3
- Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Ther Adv Gastroenterol. 2013 Jan;6(1):39–51. doi: 10.1177/1756283X12459294
- Office of Dietary Supplements – Probiotics [Internet]. [cited 2024 Aug 7]. Available from: https://ods.od.nih.gov/factsheets/Probiotics-HealthProfessional/
- Na X, Kelly C. Probiotics in Clostridium difficile Infection. J Clin Gastroenterol. 2011 Nov;45(Suppl):S154–8. doi: 10.1097/MCG.0b013e31822ec787
- Neyrinck AM, Rodriguez J, Zhang Z, Seethaler B, Mailleux F, Vercammen J, et al. Noninvasive monitoring of fibre fermentation in healthy volunteers by analyzing breath volatile metabolites: lessons from the FiberTAG intervention study. Gut Microbes. 13(1):1–16. doi: 10.1080/19490976.2020.1862028
- Neyrinck AM, Rodriguez J, Zhang Z, Nazare JA, Bindels LB, Cani PD, et al. Breath volatile metabolome reveals the impact of dietary fibres on the gut microbiota: Proof of concept in healthy volunteers. eBioMedicine. 2022 May 10;80:104051. doi: 10.1016/j.ebiom.2022.104051
- Rezaie A, Buresi M, Lembo A, Lin H, McCallum R, Rao S, et al. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. Am J Gastroenterol. 2017 May;112(5):775–84. doi: 10.1038/ajg.2017.46
Catch up on the presentations from the Breath Biopsy Conference 2024

Microbiome Content Pack: exclusive content on how breath analysis can be used for gut microbiome research