Identifying Confident Breath Biomarkers for a Potential Silicosis Test Through the Breath Biopsy VOC Atlas®
Published on: 28 Apr 2025
What is silicosis?
Silicosis is a chronic lung disease characterized by scarring of the lungs (pulmonary fibrosis) caused by inhaling large amounts of crystalline silica dust over a long period of time. This primarily affects construction workers and people working in mines. Of particular concern is the use of artificial stones, which can contain very high amounts of crystalline silica, which can cause a particularly aggressive and fast-developing form of silicosis. In the early stages, silicosis symptoms are mild, making diagnosis difficult. During the later stages of the disease, the lung scarring is more severe, producing a variety of symptoms such as coughing and shortness of breath. Currently, silicosis diagnosis is often during these later stages of the disease due to the lack of biomarkers that can be used to detect it early. As silicosis is irreversible, it is important to be able to diagnose it early and to distinguish it from other causes of lung damage. Silicosis is caused by exposure to a harmful substance similar to asbestosis, which results from exposure to asbestos fibers, however telling the difference between the two can be challenging. As there is no specific test just for silicosis, testing for silicosis in the lungs involves a variety of tests, including breathing into a spirometer to test lung function, chest X-rays and/or CT scans to check for visible signs of scarring, and bronchoscopy to obtain samples of lung fluid and tissue for analysis. The specific patterns of lung damage, and patient exposure history can assist clinicians to work out whether the cause of the scarring is silicosis.
The need for better biomarkers:
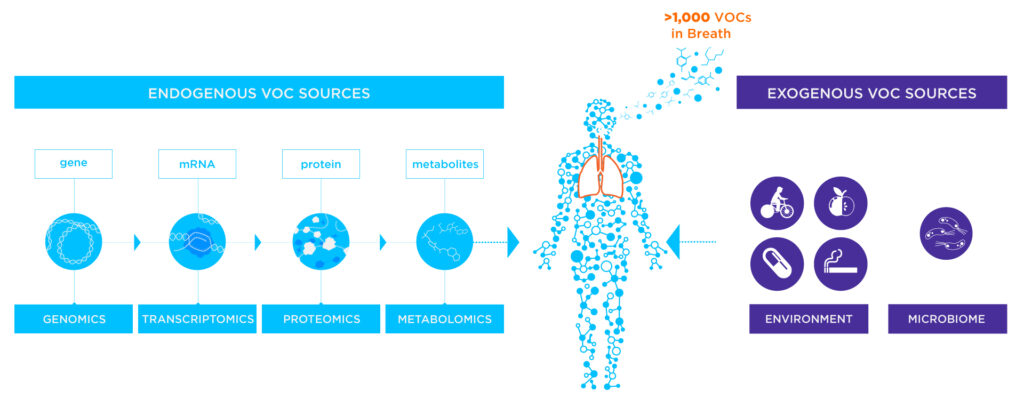
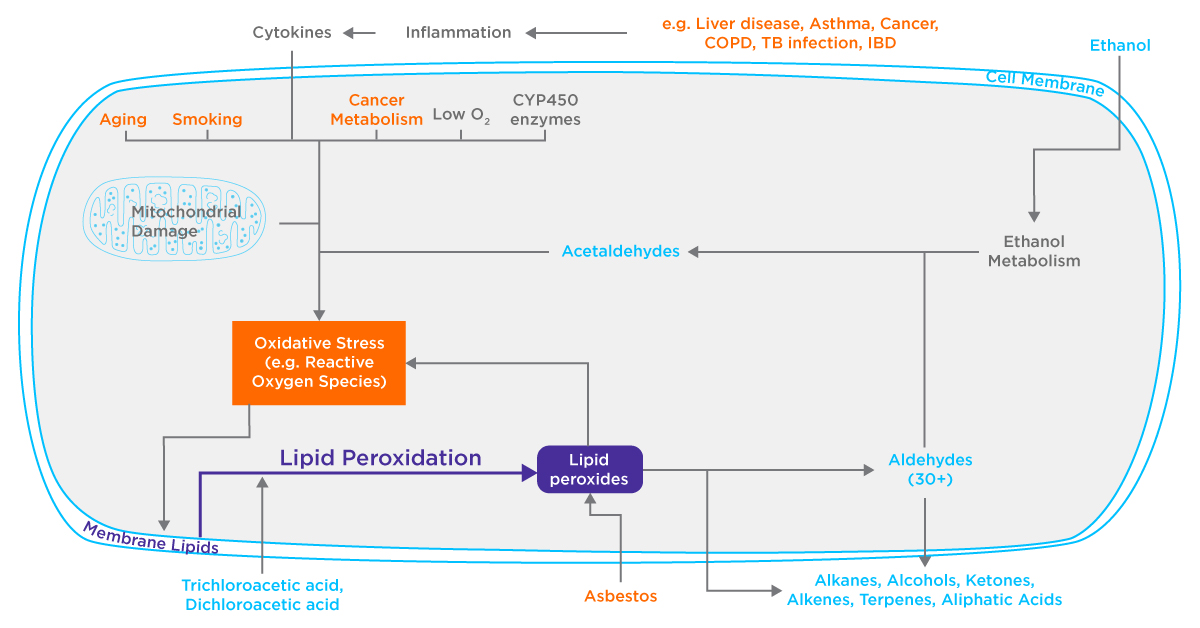
A few biomarkers for silicosis detection have been trialed previously, however, these have not achieved adequate performance to be used in the clinic. Markers such as club cell protein 16 (CC16) have been trialed previously with promising results, however, this requires a blood or BAL test to measure and is thought to be related to the proportion of healthy lung tissue, rather than silicosis specifically, so is unlikely to be able to serve as a specific biomarker for this form of lung damage (1). Exhaled breath is a non-invasive alternative to other sampling mediums, and contains volatile organic compounds (VOCs) originating as products of the body’s metabolism (endogenous VOCs) or from external sources such as diet, occupational exposure, and environmental exposure (exogenous VOCs). VOCs that are commonly detectable in exhaled breath include benzene, toluene, ethylbenzene, and xylenes (BTEX), which are related to hazardous exposures. Other exogenous VOCs could therefore originate directly from, and be used to assess, whether a patient has been exposure to a hazardous substance such as crystalline silica dust. In addition, endogenous VOCs, released from airway tissues in response to a hazardous exposure, including those relating to internal processes such as oxidative stress, lipid peroxidation, and inflammation, could be biomarkers of the detrimental downstream effects of exposure. This means that unique patterns of breath VOCs have the potential to act as biomarker assays for conditions such as silicosis. In order to identify VOCs that could serve as biomarkers for silicosis and crystalline silica dust exposure, a literature review was conducted, and a comparison to our Breath Biopsy VOC Atlas® was performed.
Using the VOC Atlas for silicosis biomarker selection
We conducted a literature review (following a PRISMA format) on VOCs associated with silicosis. The search terms used were (silicosis) AND ((VOC) OR (Volatile organic compound) OR (breathomics)). This produced four results, of which all were taken forward as being relevant based on their abstracts (2–5). From these, zero were excluded (either due to use of eNOSE, not making comparisons between silicosis and healthy, or due to the use of exhaled breath condensate). In total from these four papers, 46 VOCs associated with silicosis were identified. As the compound identifications were tentative in most of these papers (resulting from matching to e.g. NIST databases), higher confidence was given to compounds independently identified in more than one paper. In comparison to the VOC Atlas, 28 of these VOCs were in common.
Styrene was shared between three papers, and is found in the VOC Atlas and therefore known to commonly appear in the breath. Although present in small amounts in some foods such as nuts, styrene is mostly a synthetic chemical that is produced to make rubber, plastic, insulation, fiberglass, and more (6). Therefore, it is unsurprising that styrene would be associated with the breath of those with occupational exposure and silicosis. In the literature, styrene has been seen to be elevated in the breath of patients with ovarian cancer (7). Common to two of the papers in the literature review and also in the Atlas is m-xylene, also known as Benzene, 1,3-dimethyl-. Although also seen in foods such as parsley, m-xylene is commonly associated with manufacturing, and synthetic products such as paint, and cleaning products (8). Phthalic anhydride was seen in the breath of silicosis patients in two papers, however, is not currently in the VOC Atlas. Similarly to the other VOCs, phthalic anhydride is associated with the plastics industry, as it serves as an intermediate for various resins, dyes, pigments, and more – with occupational asthma being reported in production workers who working with plastic resins containing phthalic anhydride (9).
It is unclear whether these three VOCs observed in the majority of the papers in the breath of silicosis patients may arise primarily from the exposure to silica dust itself, or whether the damage caused and silicosis scarring results in a changed lung environment that allows certain exposure compounds to be excreted slower or absorb more readily into the respiratory system from inhaled air. Several of the other VOCs identified were only present in one paper, but were in the Atlas, are commonly associated with lipid peroxidation as a result of inflammation such as acetone, acetaldehyde, and nonanal (10,11). Lipid peroxidation appears to contribute to exhaled VOC profiles in many diseases, however as specific VOCs involved seem to vary by context, and different lipid compositions and redox enzymes are present in different cell types, a unique set of VOC lipid peroxidation products may signify different causes of the inflammatory response. Combined with a potentially unique signature of exogenous VOCs arising from exposure, unique breath signatures could be used to diagnose silicosis.
Conclusion
Detecting silicosis early is challenging due to a lack of reliable biomarkers, and a late showing of non-specific respiratory symptoms that are difficult to differentially diagnose. Airway inflammation is a central process in chronic respiratory diseases like cystic fibrosis, asthma, COPD, and lung cancer, but could offers potential breath-based biomarkers alongside exposure-related compounds for early, non-invasive detection of silicosis. In order to support breath biomarker development, Owlstone Medical has developed the Breath Biopsy VOC Atlas, a centralized database that offers information on identified and quantified VOCs, as well as valuable references in multiple disease areas.
The Breath Biopsy VOC Atlas offers a robust resource for identifying and developing breath-based biomarkers for diseases like silicosis. If you are interested in exploring breath-based biomarkers for exposure-related diseases such as silicosis or would like to learn more about potential volatile biomarkers that are generated in the body and found in the breath, you can now create an account to access to the VOC Atlas and contact us to learn more about how we can support your research.
References
- Naha N, Muhamed JCJ, Pagdhune A, Sarkar B, Sarkar K. Club cell protein 16 as a biomarker for early detection of silicosis. Indian J Med Res. 2020 Apr;151(4):319–25. doi: 10.4103/ijmr.IJMR_1799_18
- Yi Z, Dong S, Wang X, Xu M, Li Y, Xie L. Exploratory study on noninvasive biomarker of silicosis in exhaled breath by solid-phase microextraction–gas chromatography–mass spectrometry analysis. Int Arch Occup Environ Health. 2023 Aug 1;96(6):857–68. doi: 10.1007/s00420-023-01971-y
- León-Jiménez A, Mánuel JM, García-Rojo M, Pintado-Herrera MG, López-López JA, Hidalgo-Molina A, et al. Compositional and structural analysis of engineered stones and inorganic particles in silicotic nodules of exposed workers. Particle and Fibre Toxicology. 2021 Nov 22;18(1):41. doi: 10.1186/s12989-021-00434-x
- Hall S, Stacey P, Pengelly I, Stagg S, Saunders J, Hambling S. Characterizing and Comparing Emissions of Dust, Respirable Crystalline Silica, and Volatile Organic Compounds from Natural and Artificial Stones. Annals of Work Exposures and Health. 2022 Mar 1;66(2):139–49. doi: 10.1093/annweh/wxab055
- Jalali M, Zare Sakhvidi MJ, Bahrami A, Berijani N, Mahjub H. Oxidative Stress Biomarkers in Exhaled Breath of Workers Exposed to Crystalline Silica Dust by SPME-GC-MS. J Res Health Sci. 2016;16(3):153–61.
- PubChem. Styrene [Internet]. [cited 2025 Feb 5]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/7501
- Amal H, Shi DY, Ionescu R, Zhang W, Hua QL, Pan YY, et al. Assessment of ovarian cancer conditions from exhaled breath. International Journal of Cancer. 2015;136(6):E614–22. doi: 10.1002/ijc.29166
- PubChem. m-Xylene [Internet]. [cited 2025 Feb 5]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/7929
- PubChem. Phthalic anhydride [Internet]. [cited 2025 Feb 5]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/6811
- Filipiak W, Mochalski P, Filipiak A, Ager C, Cumeras R, Davis CE, et al. A Compendium of Volatile Organic Compounds (VOCs) Released By Human Cell Lines. Current Medicinal Chemistry. 23(20):2112–31.
- Calenic B, Miricescu D, Greabu M, Kuznetsov AV, Troppmair J, Ruzsanyi V, et al. Oxidative stress and volatile organic compounds: interplay in pulmonary, cardio-vascular, digestive tract systems and cancer. Open Chemistry. 2015 Jan 1;13(1). doi: 10.1515/chem-2015-0105