The Link Between Inflammation and Cancer
Published on: 21 Oct 2024
Inflammation is a process in the immune system’s response to infection and injury. When inflammation occurs in the body, many different immune cells may be involved. These cells release various substances called inflammatory mediators, which include the hormones histamine and bradykinin. These hormones cause the blood vessels in the tissue to dilate, allowing more blood to reach the injured tissue. This is why inflamed areas can turn red and feel hot. The increased blood flow also allows more immune cells to be carried to the injured tissue, where they help with the healing process. Both bradykinin and histamine can irritate nerves and therefore cause pain signals to be sent to the brain (1).
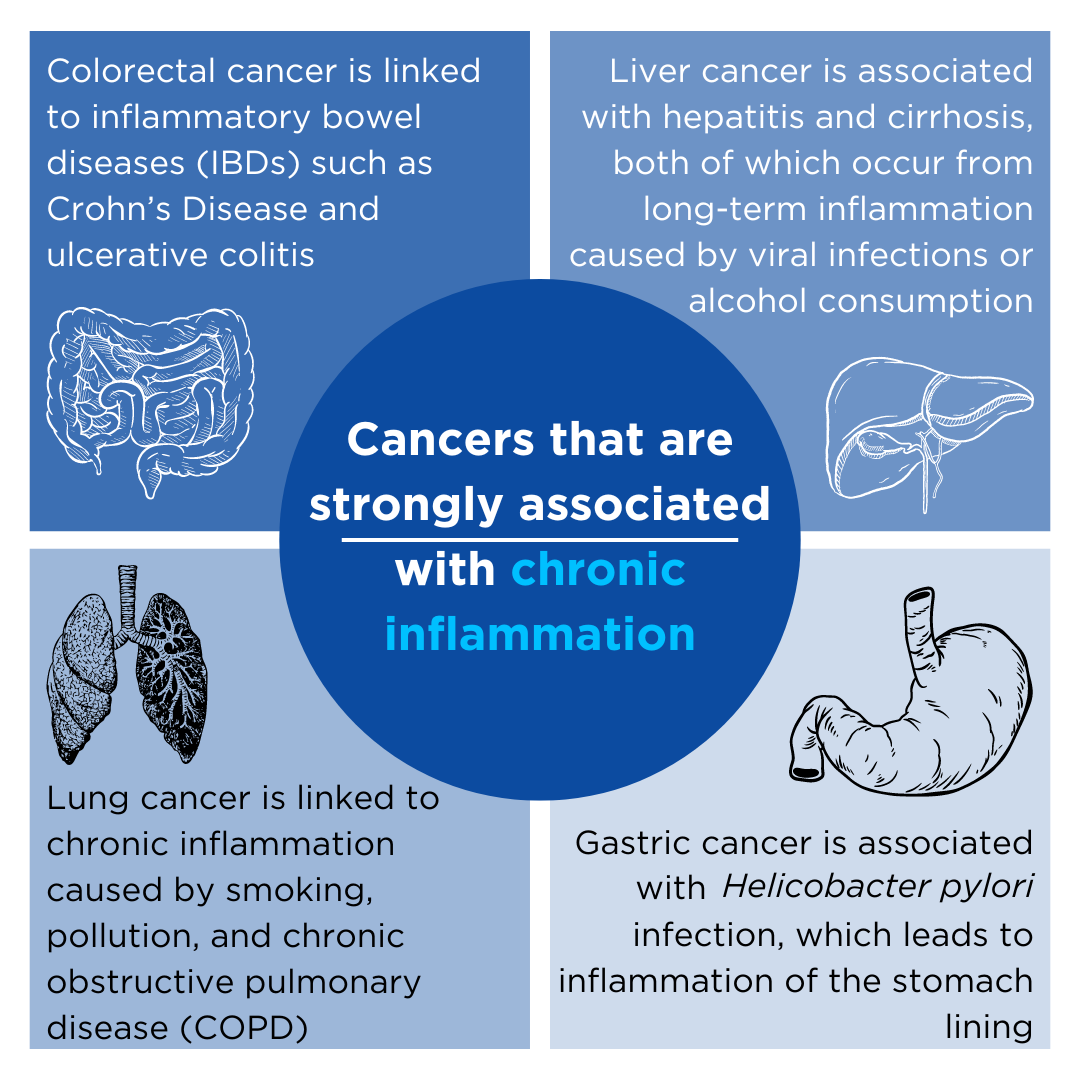
Inflammation caused by a small cut or infection like the flu is known as acute inflammation and may last for a few hours to a few days. Chronic inflammation is when this response continues over a long period of time, even in the absence of a genuine threat. For example, in arthritis, inflammatory cells attack the tissues in the joints, which leads to inflammation and damage to the joints (2). Chronic inflammation in the body can have many negative impacts on health, in particular, chronic inflammation has been associated with the development and progression of various types of cancer.
The mechanisms that link inflammation and cancer are complex and varied including interactions between immune cells and signaling molecules that can promote tumor growth and metastasis. Detecting signs of chronic inflammation in the body would therefore be clinically useful, both to diagnose and monitor patients and for clinical research purposes.
Volatile organic compounds (VOCs) are byproducts of the metabolic processes altered by inflammation and cancer. As these compounds are volatile, they can be detected and measured in exhaled breath. Breath analysis can therefore offer a non-invasive way of detecting cancer earlier and monitoring disease progression through the detection of inflammatory markers.
The Role of Inflammation in Cancer Development
Chronic inflammation contributes to carcinogenesis through several mechanisms, including:
DNA Damage
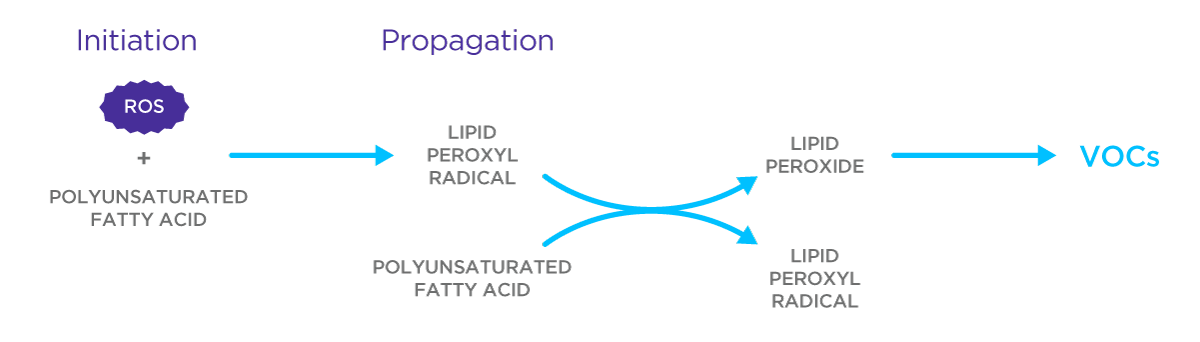
Lipid peroxidation is a result of oxidative stress within cells, which can be caused by inflammation. Our body has an intrinsic antioxidant defense, which protects us from the effects of damaging chemicals known as reactive oxygen species (ROS). In stressed cells caused by inflammation, a lack of antioxidant defense leads to an increase in ROS which can attack other components in the cell including DNA, proteins, and lipids. DNA mutations caused by ROS can contribute to the initiation of cancer (3).
Altered Cell Proliferation
Chronic inflammation is associated with the release of growth factors such as tumor necrosis factor-alpha (TNF-α) and interleukins (IL-6). These molecules can stimulate the proliferation of both immune and epithelial cells, which increases the likelihood of genetic mutations occurring that can lead to cancer development (4).
Promotion of Angiogenesis
Inflammatory cytokines can promote the formation of new blood vessels, known as angiogenesis. Angiogenesis plays a role in the growth of cancer as tumours need a blood supply if they are to grow beyond a few millimetres in size. Tumors can cause this blood supply to happen by giving off chemical signals that stimulate angiogenesis. The resulting new blood vessels feed tumors with oxygen and nutrients, allowing the tumor to grow and metastasize (5).
Immune System Invasion
Cancer cells can manipulate the immune system to create an immunosuppressive microenvironment. Chronic inflammation facilitates the recruitment of regulatory T cells and suppressor cells that can inhibit the anti-tumor immune response, increasing the likelihood of cancer metastasis (6).
VOCs as Biomarkers for Inflammation and Cancer
Exhaled breath contains hundreds of different VOCs, many of which are products of oxidative stress, which is especially prevalent during chronic inflammation. These VOCs can therefore serve as biomarkers of disease, as they can reflect metabolic alterations that arise due to inflammation and cancer.
When inflammation occurs, the increased production of ROS leads to more oxidative damage, including lipid peroxidation – the oxidative degradation of lipids in cell membranes. This process generates VOCs, such as alkanes, aldehydes, and ketones. These are examples of compounds you can find in our Breath Biopsy VOC Atlas®, an expanding reference database of the chemically identified, confirmed compounds detectable in human breath. Find out more about our VOC Atlas here. The types and concentrations of VOCs in exhaled breath can change in response to different inflammatory processes and the presence of cancer (7).
Studies have shown that specific VOCs are elevated in the breath of individuals with specific types of cancer. For example:
- Lung cancer = VOCs such as alkanes and benzene derivatives are frequently found to be elevated in the breath of lung cancer patients (8).
- Colorectal cancer = aldehydes (specifically decanal) have been found in higher concentrations in the breath of patients with colorectal cancer (9).
- Breast cancer = VOCs such as cyclopentanone, phenol, and ethylene carbonate have been identified as potential biomarkers of breast cancer (10).
The inflammation seen in cancer produces unique VOC signatures which reflect the interactions between cancer cells, immune cells, and the surrounding microenvironment. Under chronic inflammatory conditions, tumor cells undergo ‘metabolic reprogramming’, which can alter the types of VOCs they emit (11). This metabolic reprogramming includes increased glycolysis, known as the Warburg effect, and heightened lipid metabolism, both of which produce distinct VOCs that can be measured in exhaled breath (12).
Also, immune cells involved in the inflammatory response, such as macrophages and neutrophils, can contribute to VOC production. For example, macrophages can release nitric acid (NO) and related nitrogen species, which can generate nitrogen-containing VOCs (13).
How can Owlstone Medical help?
VOCs that originate from cancer-specific metabolism and inflammatory processes can readily enter our lungs and be exhaled from the body in breath. Breath is a virtually inexhaustible resource, with large volumes able to be collected at frequent intervals, meaning breath analysis can provide an almost real-time longitudinal analysis of VOCs. The non-invasive nature of breath analysis makes it more attractive than techniques often used to observe and diagnose cancer such as biopsies, where damage can occur to the surrounding tissue and can be uncomfortable for the patient.
Owlstone Medical is the world leader in breath research for the early detection of disease, a factor that is extremely important in the fight against cancer. We are here to help you include breath analysis in your research. Breath Biopsy OMNI can provide everything you may need to start or continue using breath analysis, as well as expert advice from our team of scientists. You can cross-check your data against our VOC Atlas, to better understand how VOCs behave in a healthy population and confidently validate your cancer biomarkers.
References
- Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, et al. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2017 Dec 14;9(6):7204–18. doi: 10.18632/oncotarget.23208
- Schett G. Resolution of inflammation in arthritis. Semin Immunopathol. 2019 Nov;41(6):675–9. doi: 10.1007/s00281-019-00768-x
- Kay J, Thadhani E, Samson L, Engelward B. Inflammation-Induced DNA Damage, Mutations and Cancer. DNA Repair (Amst). 2019 Nov;83:102673. doi: 10.1016/j.dnarep.2019.102673
- Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011 Mar 4;144(5):646–74. doi: 10.1016/j.cell.2011.02.013
- Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011 May 19;473(7347):298–307. doi: 10.1038/nature10144
- Sica A, Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest. 2007 May;117(5):1155–66. doi: 10.1172/JCI31422
- Filipiak W, Sponring A, Filipiak A, Ager C, Schubert J, Miekisch W, et al. TD-GC-MS analysis of volatile metabolites of human lung cancer and normal cells in vitro. Cancer Epidemiol Biomarkers Prev. 2010 Jan;19(1):182–95. doi: 10.1158/1055-9965.EPI-09-0162
- Phillips M, Cataneo RN, Cummin ARC, Gagliardi AJ, Gleeson K, Greenberg J, et al. Detection of lung cancer with volatile markers in the breath. Chest. 2003 Jun;123(6):2115–23. doi: 10.1378/chest.123.6.2115
- Altomare DF, Di Lena M, Porcelli F, Trizio L, Travaglio E, Tutino M, et al. Exhaled volatile organic compounds identify patients with colorectal cancer. Br J Surg. 2013 Jan;100(1):144–50. doi: 10.1002/bjs.8942
- Zhang Y, Guo L, Qiu Z, Lv Y, Chen G, Li E. Early diagnosis of breast cancer from exhaled breath by gas chromatography‐mass spectrometry (GC/MS) analysis: A prospective cohort study. J Clin Lab Anal. 2020 Nov 4;34(12):e23526. doi: 10.1002/jcla.23526
- Xia L, Oyang L, Lin J, Tan S, Han Y, Wu N, et al. The cancer metabolic reprogramming and immune response. Mol Cancer. 2021 Feb 5;20:28. doi: 10.1186/s12943-021-01316-8
- Ward PS, Thompson CB. Metabolic reprogramming: a cancer hallmark even warburg did not anticipate. Cancer Cell. 2012 Mar 20;21(3):297–308. doi: 10.1016/j.ccr.2012.02.014
- Zhuang JC, Wogan GN. Growth and viability of macrophages continuously stimulated to produce nitric oxide. Proc Natl Acad Sci U S A. 1997 Oct 28;94(22):11875–80. doi: 10.1073/pnas.94.22.11875