Smelling Cancer: How Medical Detection Dogs Can Inspire Breath Analysis
Published on: 9 Sep 2024
For thousands of years, dogs have been human companions, serving as both diligent workers and loyal friends. One of their most impressive qualities is their highly sensitive sense of smell. Some species can sniff out truffles and others can be trained to detect drugs, weapons, and bombs. The power of a dog’s olfactory system even extends to the detection of human diseases. In 1989, a woman took a trip to the doctors to discuss a mole that her dog would continuously sniff and bite at, only to discover it was a malignant melanoma, a type of cancer (1). Since this event, it has been observed that dogs can smell a range of cancer subtypes, as well as a range of other diseases, including malaria, Parkinson’s disease, and epilepsy (2–5).
The most likely explanation is that the olfactory receptors of dogs are detecting volatile organic compounds (VOCs). VOCs are produced by metabolic processes and are transported around the body and into the lungs via blood vessels. These can be released as waste products alongside gases like carbon dioxide when we breathe out, or as sweat and in urine. Pathological processes can alter the VOC profile by causing a change in the concentration of the VOCs normally produced in the cell or by synthesizing disease-specific compounds. These differences in VOC signatures between healthy and diseased states could therefore allow dogs to recognize disease.
Just like dogs, there are some occasions when humans can also smell disease. For example, when diabetes is not kept under control, ketoacidosis can occur. This produces large amounts of acetone and causes a characteristic fruity odor on the breath (6). But why are dogs 10,000 to 100,000 times better at differentiating smells than humans (7)? Dogs have huge numbers of olfactory receptors and a high proportion of active to inactive genes encoding these receptors, increasing the diversity of compounds that they can detect. The shape of the canine snout is also optimized to increase airflow in the nasal cavity (8).
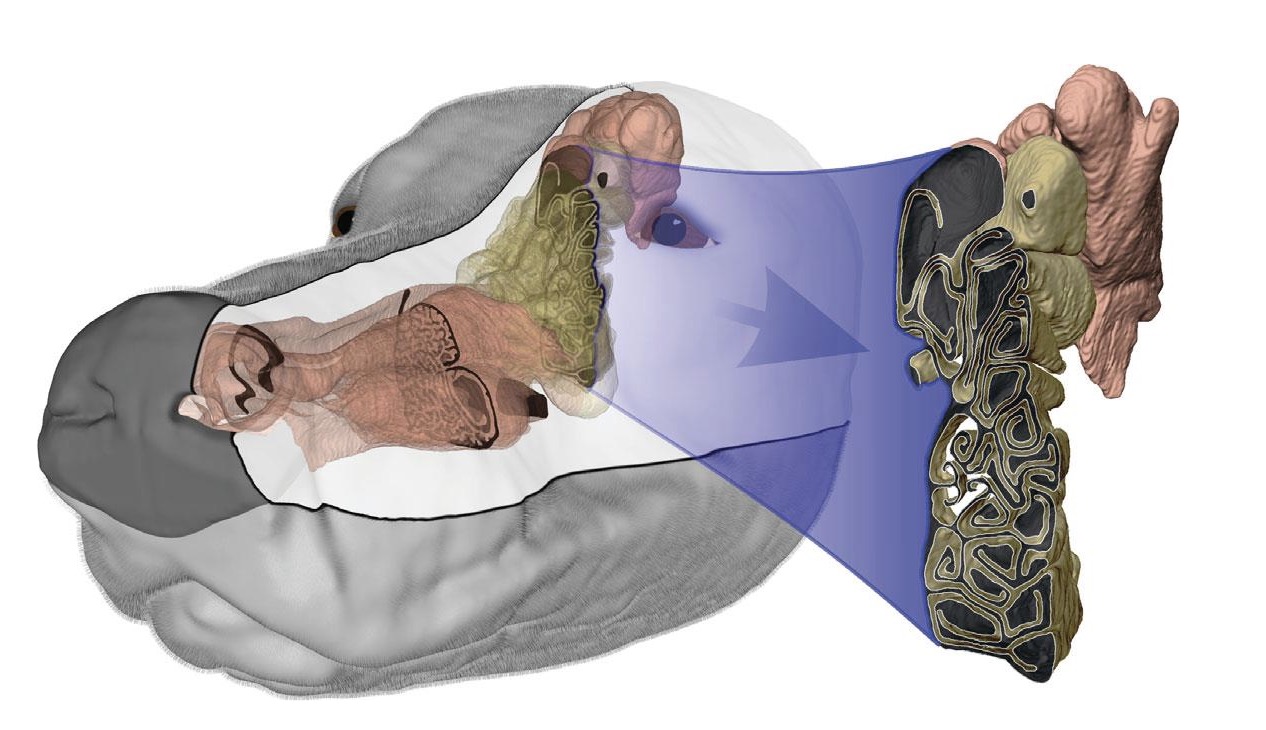
3D model of a dog’s olfactory senses, image by NNDDA Judge Chris Vaughn (9).
Disease case studies
Cancer
Metabolic reprogramming is a key feature of cancer that aids its survival and proliferation. The upregulation of certain processes can alter the VOC profile of the cells compared to non-cancerous cells and hence the composition of excreted VOCs. In 2021, Feil et al. used a combination of breath and urine samples to investigate the ability of dogs to detect lung cancer (7). A high overall detection rate of 97.6% was achieved when using both urine and breath samples, with a 78% accuracy for breath samples alone. A study by McCulloch et al. demonstrated even more sensitive detection of lung cancer by dogs from breath, with a value of 0.99 for both specificity and sensitivity (10). However, the specific VOCs that allow dogs to detect cancer from breath samples have yet to be conclusively determined. Identifying these VOCs could allow for the development of breath tests for lung cancer that maintain the non-invasiveness of canine screening but are validated for clinical use, whilst also increasing our understanding of the disease. At Owlstone Medical, we are working on a longitudinal study known as EVOLUTION which aims to develop non-invasive breath tests for lung cancer screening and early detection.
Dogs have also been demonstrated to detect other subtypes of cancer through breath samples. McCulloch et al. produced a sensitivity of 0.88 and a specificity of 0.98 for the detection of breast cancer from breath samples by dogs (10). Sonoda et al. also demonstrated that dogs were able to detect colorectal cancer with a sensitivity of 0.91 compared to conventional diagnosis by colonoscopy, and a specificity of 0.99 (11).
Infectious diseases
During infections, the body’s VOC profile can be altered. VOCs can be excreted directly as a pathogen’s metabolites or through host immune responses to that pathogen. One study by Devillier et al. demonstrated the ability of dogs to detect the presence of SARS-CoV-2 infection in exhaled breath and axillary sweat samples (12). The dogs were able to detect PCR-positive patients from breath samples with a sensitivity of 83.1%, and a specificity of 88.6%. There was no difference in the detection of disease in breath compared to sweat samples, indicating a shared VOC pattern between the two.
Stress and neurological disorders
Stress causes a range physiological response in the body, many of which are mediated through changes to metabolism, and therefore alter the VOC profile. A 2022 study by Wilson et al. demonstrated that physiological changes induced by psychological stress could be detected by dogs in sweat/breath samples (13). Dogs were able to distinguish the stressed state from the calm state with a 93.75% accuracy. This information has important implications for post-traumatic stress disorder (PTSD) service dogs, which are important for detecting and aiding people having stress episodes. A 2024 study by Kiiroja et al. demonstrated that dogs could detect differences in the breath by people with PTSD when they experience distress associated with past trauma (14). The dogs were able to detect the stressed state on breath samples with 81% accuracy, with a 90% accuracy when discriminating between control and stressed samples.
What does this mean for breath analysis?
Numerous studies across a range of diseases have shown that dogs can detect disease from exhaled breath samples, providing a strong basis for using breath analysis as a non-invasive disease screening method. These studies highlight that there are genuine composition changes that can be picked up by dogs’ highly sensitive noses. Gas chromatography-mass spectrometry (GC-MS), which can used for the high-accuracy analysis of compounds in breath testing, is also highly sensitive to VOCs, able to detect compounds into the range of parts per trillion.
Owlstone Medical’s Breath Biopsy technology standardizes the breath sampling and analysis processes, providing results with enhanced reliability when compared to canine screening, including the collection and analysis of odorless VOCs. We also achieve high sensitivity of VOC detection due to our robust breath sample collection techniques that concentrate a wide range of VOCs from a large volume of exhaled breath to identify VOCs that are at low concentrations.
Breath analysis provides a mechanism to identify and quantify the disease-specific VOCs exhaled on breath, something not possible with dogs. Using VOCs of known identity to detect disease improves the reliability and repeatability of the detection of disease and can allow the validation of specific markers for translation into clinical tests that can be properly interpreted. Through our Breath Biopsy OMNI platform, we offer services for the accurate identification and quantification of VOC biomarkers at high sensitivity and can support the development of point-of-care breath analysis tests for specific diseases.
To learn more about how breath analysis can be used for the studying and diagnosis of disease, explore our disease case studies, or contact us using the link below.
References
- Williams H, Pembroke A. Sniffer dogs in the melanoma clinic? Lancet Lond Engl. 1989 Apr 1;1(8640):734. doi: 10.1016/s0140-6736(89)92257-5
- Pellin MA, Malone LA, Ungar P. The use of sniffer dogs for early detection of cancer: a One Health approach. American Journal of Veterinary Research. 2024 Jan 1;85(1). doi: 10.2460/ajvr.23.10.0222
- Guest C, Pinder M, Doggett M, Squires C, Affara M, Kandeh B, et al. Trained dogs identify people with malaria parasites by their odour. Lancet Infect Dis. 2019 Jun 1;19(6):578–80. doi: 10.1016/S1473-3099(19)30220-8
- Gao CQ, Wang SN, Wang MM, Li JJ, Qiao JJ, Huang JJ, et al. Sensitivity of Sniffer Dogs for a Diagnosis of Parkinson’s Disease: A Diagnostic Accuracy Study. Mov Disord Off J Mov Disord Soc. 2022 Sep;37(9):1807–16. doi: 10.1002/mds.29180
- Catala A, Grandgeorge M, Schaff JL, Cousillas H, Hausberger M, Cattet J. Dogs demonstrate the existence of an epileptic seizure odour in humans. Sci Rep. 2019 Mar 28;9(1):4103. doi: 10.1038/s41598-019-40721-4
- Sha MS, Maurya MR, Shafath S, Cabibihan JJ, Al-Ali A, Malik RA, et al. Breath Analysis for the In Vivo Detection of Diabetic Ketoacidosis. ACS Omega. 2022 Jan 24;7(5):4257–66. doi: 10.1021/acsomega.1c05948
- Feil C, Staib F, Berger MR, Stein T, Schmidtmann I, Forster A, et al. Sniffer dogs can identify lung cancer patients from breath and urine samples. BMC Cancer. 2021 Aug 13;21(1):917. doi: 10.1186/s12885-021-08651-5
- Pirrone F, Albertini M. Olfactory detection of cancer by trained sniffer dogs: A systematic review of the literature. J Vet Behav. 2017 May 1;19:105–17. doi: 10.1016/j.jveb.2017.03.004
- NNDDA. Factors affecting K9 Olfaction [Internet]. National Narcotic Detector Dog Association. 2020 [cited 2024 Aug 16]. Available from: https://nndda.org/factors-affecting-k9-olfaction/
- McCulloch M, Jezierski T, Broffman M, Hubbard A, Turner K, Janecki T. Diagnostic Accuracy of Canine Scent Detection in Early- and Late-Stage Lung and Breast Cancers. Integr Cancer Ther. 2006 Mar 1;5(1):30–9. doi: 10.1177/1534735405285096
- Sonoda H, Kohnoe S, Yamazato T, Satoh Y, Morizono G, Shikata K, et al. Colorectal cancer screening with odour material by canine scent detection. Gut. 2011 Jun 1;60(6):814–9. doi: 10.1136/gut.2010.218305
- Devillier P, Gallet C, Salvator H, Lecoq-Julien C, Naline E, Roisse D, et al. Biomedical detection dogs for the identification of SARS-CoV-2 infections from axillary sweat and breath samples**. J Breath Res. 2022 Apr;16(3):037101. doi: 10.1088/1752-7163/ac5d8c
- Wilson C, Campbell K, Petzel Z, Reeve C. Dogs can discriminate between human baseline and psychological stress condition odours. PLoS ONE. 2022 Sep 28;17(9):e0274143. doi: 10.1371/journal.pone.0274143
- Kiiroja L, Stewart SH, Gadbois S. Can scent-detection dogs detect the stress associated with trauma cue exposure in people with trauma histories? A proof-of-concept study. Front Allergy. 2024 Mar 28;5:1352840. doi: 10.3389/falgy.2024.1352840