A Proof-of-Principle Study in Propionic Acidemia – Discover Breath Biopsy® in Action
This study investigated the VOCs present in breath of participants with propionic acidemia, and identified correlations with biochemical characteristics of the disease
| Publication information: Oleg Shchelochkov, Huw Davies, Robert P. Mohney, Ace Hatch, Owen Birch, Susan Ferry, Carol Van Ryzin, Camryn Hall, Samantha McCoy, Gerard Vockley, Mickey J.M. Kuo, Irini Manoli, Jennifer Sloan, and Charles P. Venditti. Breath biopsy in inborn errors of metabolism: A proof-of-principle study in propionic acidemia.
Disease Area: Propionic acidemia. Application: Biomarker development. Sample Medium: Exhaled breath. Analysis Approach: Breath Biopsy® OMNI® assay, TD-GC-MS. Summary:
|
Introduction – Propionic Acidemia
In biochemical genetics, volatile chemicals have played a diagnostic role in various disorders, mostly related to abnormal amino acid metabolism. For example, a ‘sweet’ smell of sotolone is detected in maple syrup urine disease (1). Many examples of diagnostic volatile chemicals are linked to disorders of impaired oxidation of branched-chain amino acids (BCAA), given their low molecular weight and complex catabolism which has the potential to generate volatile organic compounds (VOCs) (2).
Disorders of BCAA oxidation are a group of inborn errors of metabolism that have clinical manifestations ranging from life-threatening to benign biochemical traits (2). Many of these disorders have limited or no means to monitor their clinical course in the outpatient setting, stratify their severity, or detect metabolic decompensations.
Propionic acidemia is an example of a severe disorder linked to the BCAA oxidation pathway and is characterized by the deficient activity of propionyl-CoA carboxylase. Some intermediates in the BCAA pathway have properties of VOCs that can undergo additional chemical modifications leading to the formation of additional VOCs such as aldehydes, ketones, and short-chain fatty acids (3).
The detection of VOCs in exhaled breath is a promising approach that can support the diagnosis and evaluation of disease outcomes. Breath analysis is non-invasive, meaning that, unlike blood tests and biopsies, collecting a breath sample is painless and simple. Exhaled breath is an inexhaustible resource compared to other sampling methods such as blood tests as it is produced constantly from the body and can be collected in large volumes.
The compounds found in breath samples can be pre-concentrated before analysis, enabling repeated or continuous measurements to assess a patient’s condition, opening the potential for real-time monitoring. This positions breath analysis as a technique that can be used to monitor disease progression, evaluate treatment response, and detect signs of reoccurring disease. A recent study by Shchelochkov et al hypothesized that enzymatic defects in the BCAA oxidation pathway can increase VOCs, with an accumulation in exhaled breath proportionate to the severity of the underlying disorder (4).
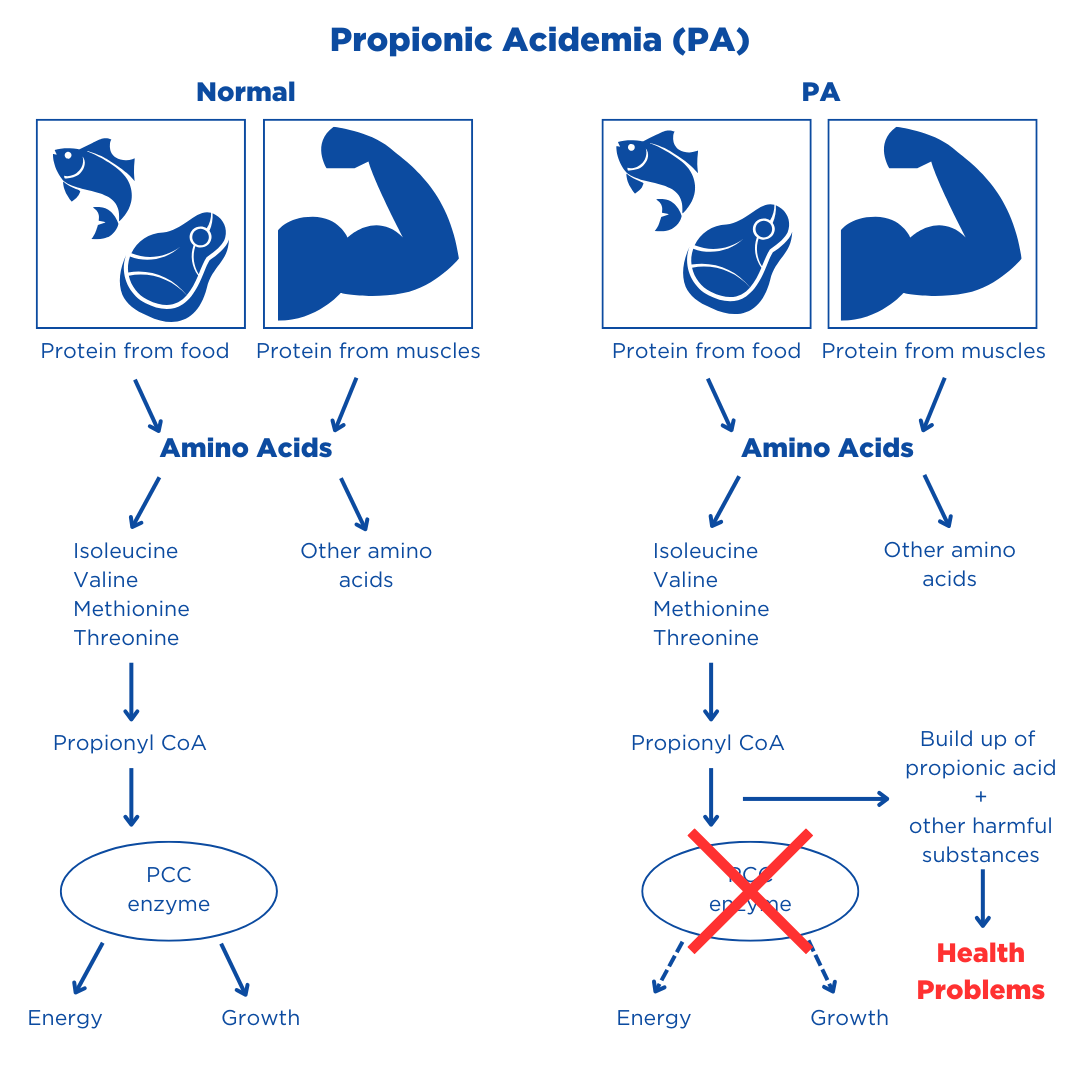
Figure 1. PA occurs when the enzyme “propionyl CoA carboxylase” (PCC) is either missing or not working properly. This enzyme’s job is to change certain amino acids so the body can use them. When this enzyme is not working, substances called glycine and propionic acid, along with other harmful substances, build up in the blood and cause problems. Adapted from Newborn Screening Info.
Methods
Participants
Five participants with propionic acidemia and five healthy controls were enrolled. Given the rarity and heterogeneity of propionic acidemia, the cohort was designed to include cases representing a range of clinical and biochemical manifestations. The five propionic acidemia participants had undergone phenotyping that included clinical, imaging, and biochemical parameters as well as in vivo whole-body 1-13C-propionate oxidation and quantitative analysis of 2-methylcitrate and propionylcarnitine in the previous NIH study (5). Plasma lactate, pyruvate, and 3-OH-propionate were measured by GC-MS in this study.
Collection of Samples for VOC Analysis
Breath samples were collected using the ReCIVA® Breath Sampler. Exhaled breath from both the upper and lower airways were sampled.
Quality Controls and Calibration Standards
An assessment of the quality of the breath sample and the volume collected was performed by Owlstone Medical.
VOC Analysis
Breath samples were analyzed at the Breath Biopsy Laboratory of Owlstone Medical, using the Breath Biopsy OMNI assay. Before the collection of data, a hypothesis-driven list of candidate VOCs likely to appear in propionic acidemia cases was submitted for targeted analysis. These compounds included those related to the metabolism of BCAAs, levocarnitine, and ketones. An unbiased analysis of TD-GC-MS from the tidal breath was performed to identify additional VOC candidates.
Candidate VOCs were then identified by matching their spectral features against VOC profiles listed in the National Institute of Standards and Technology (NIST) and Owlstone Medical’s High-Resolution Accurate Mass (HRAM) reference libraries.
Results
Unbiased Screening Identifies VOC Candidates
The TD-GC-MS analysis of tidal breath from the participants identified tentative candidates with features matching NIST and HRAM reference profiles of propionate derivatives as well as volatile aldehydes and ketones. Using a spectral comparison to NIST reference profiles, a VOC that was 45-fold higher in the propionic acidemia participants compared to healthy controls was identified as 3-pentanone.
3-Pentanone Correlates with the Clinical and Biochemical Severity of Propionic Acidemia
After confirming the identity of 3-pentanone, the abundance was compared to the biochemical and clinical outcomes in propionic acidemia. 3-Pentanone directly correlated with plasma propionylcarnitine, total 2-methylcitrate, 3-OH-propionate, lactate, and pyruvate. 3-Pentanone was also inversely correlated with whole-body in vivo oxidation of 1-13C-propionate.
Discussion
This study demonstrated that 3-pentanone is significantly elevated in propionic acidemia and appears to be linked to the underlying severity of propionic acidemia. Also, 3-pentanone was found to be significantly associated with known propionic acidemia biomarkers including propionylcarnitine, 2-methylcitrate, 3-OH-propionate, lactate, and pyruvate in blood.
Detection of 3-pentanone has been found in two previous VOC studies linking small increases to non-specific causes like liver disease, liver cirrhosis, and inflammation (6). It is thought that the level of 3-pentanone elevation in propionic acidemia stems from causes such as hepatic dysfunction. The mechanism of 3-pentanone formation remains unclear, a pathway of its formation is proposed in propionic acidemia.
It involves the formation of 3-keto-2-methylvaleric acid through the condensation of two molecules of propionyl-CoA, followed by its decarboxylation. Consistent with this hypothesis, the excretion of 3-keto-2-methylvaleric acid has been demonstrated in propionic acidemia patients (7).
Although 3-keto-2-methylvaleric acid can degrade ex vivo, this study highlights it is unlikely to be a significant source of 3-pentanone due to its low vapor pressure and low volatility. It was therefore concluded that the in vivo formation of 3-pentanone was more likely reflective of the in vivo metabolism of propionyl-CoA.
Therefore, this proof-of-principle study demonstrates that non-invasive breath sampling paired with TD-GC-MS is a promising method, capable of identifying VOCs that correlate with the clinical and biochemical parameters of propionic acidemia.
At Owlstone Medical, we have many tools and services that can incorporate breath analysis into your research, including our Breath Biopsy OMNI platform – the most advanced solution for volatile metabolite analysis in the breath. Our OMNI service allows for standardized breath collection and includes broad analysis methodologies optimized for reproducible identification and quantification of relevant metabolites. We can also provide expert support on study design, project management, and data interpretation.
Our Breath Biopsy VOC Atlas® has currently more than 200 rigorously identified VOCs, including metabolic-associated VOCs. You can sign up and gain access to the VOC Atlas here.
References
- Burke DG, Halpern B, Malegan D, McCairns E, Danks D, Schlesinger P, et al. Profiles of urinary volatiles from metabolic disorders characterized by unusual odors. Clinical Chemistry. 1983 Oct 1;29(10):1834–8. doi: 10.1093/clinchem/29.10.1834
- Manoli I, Venditti CP. Disorders of branched chain amino acid metabolism. Transl Sci Rare Dis. 2016 Nov 7;1(2):91–110. doi: 10.3233/TRD-160009
- Lehnert W, Sperl W, Suormala T, Baumgartner ER. Propionic acidaemia: clinical, biochemical and therapeutic aspects. Experience in 30 patients. Eur J Pediatr. 1994;153(7 Suppl 1):S68-80. doi: 10.1007/BF02138781
- Shchelochkov OA, Davies H, Mohney RP, Hatch A, Birch O, Ferry S, et al. Breath biopsy in inborn errors of metabolism: A proof-of-principle study in propionic acidemia. Molecular Genetics and Metabolism. 2025 Mar 1;144(3):109005. doi: 10.1016/j.ymgme.2024.109005
- Shchelochkov OA, Manoli I, Juneau P, Sloan JL, Ferry S, Myles J, et al. Severity modeling of propionic acidemia using clinical and laboratory biomarkers. Genet Med. 2021 Aug;23(8):1534–42. doi: 10.1038/s41436-021-01173-2
- Kleber A, Maurer F, Lorenz D, Wolf B, Albrecht F, Shopova T, et al. Metabolism of 3-pentanone under inflammatory conditions. J Breath Res. 2016 Sep 28;10(4):047101. doi: 10.1088/1752-7155/10/4/047101
- Bergstrøm T, Greter J, Levin AH, Steen G, Tryding N, Wass U. Propionyl-CoA carboxylase deficiency: case report, effect of low-protein diet and identification of 3-oxo-2-methylvaleric acid 3-hydroxy-2-methylvaleric acid, and maleic acid in urine. Scand J Clin Lab Invest. 1981 Apr;41(2):117–26. doi: 10.3109/00365518109092023