Breath metabolites provide fresh insights into the gut microbiome (2018)
Significant correlation between breath VOCs and intestinal microbiota
| Publication information: A. Smolinska et al. Volatile metabolites in breath strongly correlate with gut microbiome in CD patients, Analytica Chimica Acta. (2018) 1025: pp 1-11. DOI: 10.1016/j.aca.2018.03.046
Disease Area: Crohn’s disease, Gut microbiome, Gastrointestinal Application: Ongoing monitoring Sample medium: Breath Analysis approach: GC-Tof-MS Summary:
|
The gut microbiome plays a key role in establishing and maintaining a healthy metabolism. Much of the food we eat as a part of a normal diet can only be metabolized by the gut microbes, as opposed to human metabolic processes. Complex microbe-microbe interactions and microbe-host interactions in our gut release huge numbers of varied metabolites that affect our gut’s health – and the health of the rest of our body too.
Volatile organic compounds (VOCs) produced as metabolites within the gut are picked up in the bloodstream, carried to the lungs, exchanged into air and then excreted on exhaled breath. The concentrations of certain volatiles detectable on breath (such as the short chain fatty acids [SCFAs] acetate, butyrate and propionate, and alcohols like ethanol and propanol) have been proposed to vary in line with host health and disease states.
This suggests that breath VOCs could be useful for both diagnosing and monitoring gastrointestinal disorders. Developing breath tests for gastrointestinal diseases is a particularly attractive option due to the non-invasive nature of breath collection and its potential for at-home use.
Previous studies of patients with Crohn’s Disease (CD) have found that concentrations of specific breath VOC groups corresponded to the patient’s current disease state (active or remission). Metagenomic studies of patient’s fecal microbiota have found groups of microbes also varying with disease state.
This study from Smolinska et al. sought to investigate a link between these two areas and aimed to demonstrate a connection between specific volatile metabolites in exhaled breath and gut microbiota composition. According to Smolinska et al.:
“Unravelling this link is essential to increase our understanding of microbial-host interactions and enhance new leads for disease monitoring.”
Methods
68 patients with an established CD diagnosis provided 184 paired breath and fecal samples, 92 during active and 92 during inactive disease. Pyrosequencing was employed to sequence the microbiota in fecal samples. Breath samples were collected in Tedlar bags, with VOCs then transferred onto sorption tubes before analysis via GC-Tof-MS.
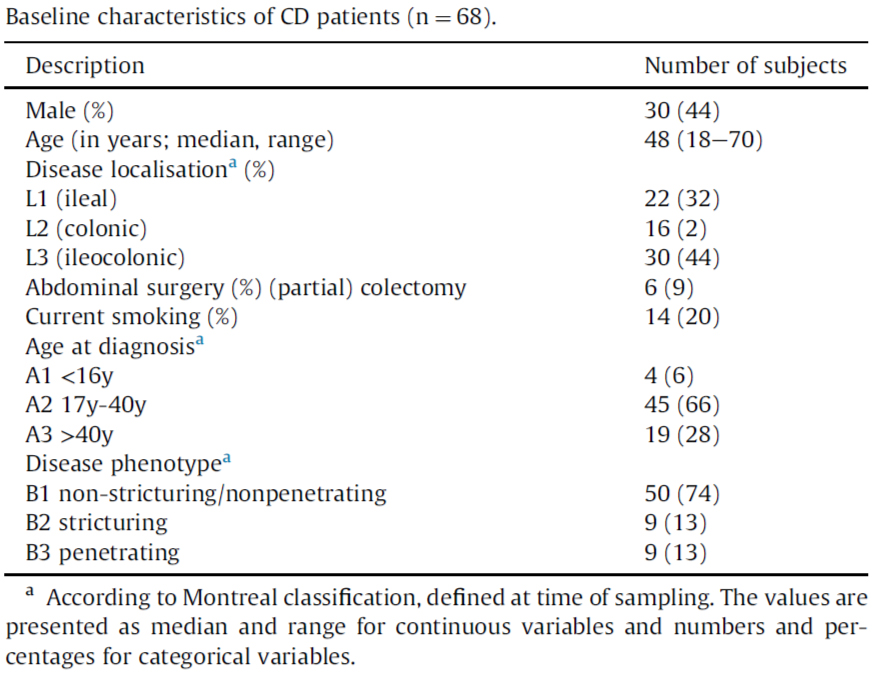
Table 1. Baseline characteristics of CD patients.
Results
From both disease state samples collected, the breath samples contained 545 different VOCs. For the purposes of canonical correlation analysis, VOCs presented in less than 20% of the samples were removed, while raw clustered fecal microbiome data were combined to the species- or genus-level taxa.
Comparing the resulting 256 VOCs and 166 bacterial taxa, Smolinska et al. found a high level of correlation: 0.90 (p-value 0.00012) and 0.89 (p-value 0.001) in inactive and active disease states, respectively.
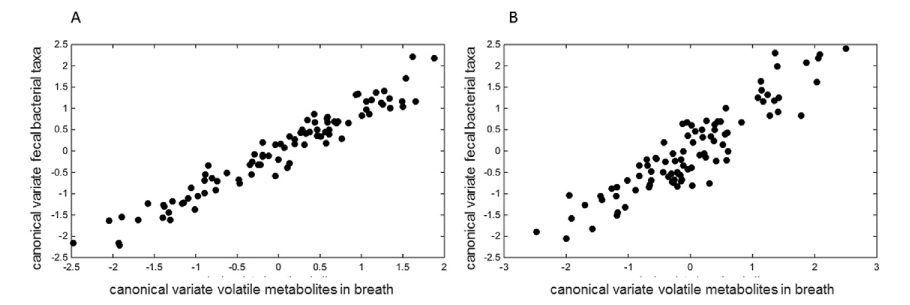
Figure 1: The canonical correlation score plot using the first canonical variates of selected sets of the most important volatile metabolites in breath (x-axis) and faecal bacterial taxa (yaxis) for: A) inactive CD patients; B) CD in active stage.
Based on sensitivity analysis, 17 breath VOCs and 17 bacterial taxa, as well as 18 VOCs and 19 bacterial taxa contributed most greatly to the correlation during the inactive and active disease state, respectively. Further correlation analysis based on these VOCs and bacterial taxa elevated results of both inactive (R= 0.96) and active (R= 0.91) disease.
Among these findings, 9 VOCs and 3 bacterial taxa overlapped between the two disease states. Tentative identities were assigned to all these significant VOC contributors to correlation – though without reference to pure chemical standards.
Discussion
Smolinska et al. conclude that this study:
“demonstrates the existence of strong, significant, relation[s] between the intestinal microbiota and volatile metabolites in exhaled breath.”
Similar to other breath studies in gastrointestinal health, SCFAs (acetate, pentanoate and propionate) were found in exhaled breath and correlated significantly with the fecal microbiota in both active and inactive CD, with slightly stronger correlation in the latter. SCFAs are formed by the gut microbiota during fermentation of non-digestible carbohydrates, with beneficial health impacts for the host.
Acetate (the most abundant SCFA in the gut) and propionate showed statistically significant correlation with Bifidobacteria and several members of the Firmicutes phylum in both inactive and active disease state. The relative abundances of SCFAs and microbial strains associated with their production were both reduced in active disease states.
Smolinska et al. also found statistically significant correlations, in the samples from patients in active disease state, between Bacteroides fragilis and Ruminococcus gnavus, and VOCs, like pentane and octane that are commonly associated with inflammation. This doesn’t necessarily mean that these bacteria produce these specific VOCs – the bacterial and VOC concentrations could instead share a common cause.
There are lots of interesting results in Smolinska et al.’s paper worthy of further investigation. However, the study did have several limitations, one being a significant correlation found between some bacteria and phenol, a known contaminant often traced to Tedlar bags.
As a result of using Tedlar bags, their breath collection also included dead space air, diluting samples. They also didn’t collect any ambient blanks or employ other methods to remove possible ambient confounding chemicals from the final VOC data set.
Another possible limitation not discussed by Smolinska et al. is whether the paired breath and fecal samples reflect the same metabolic state. Breath collected in the clinic and the submitted fecal samples collected prior at home differed up to 12 hours.
While breath provides a real-time snapshot of metabolic activity within the body, fecal analysis is more reflective of gut activity in the recent past – up to 48 hours before defecation. This could potentially lead to a drift in the actual composition of gut microbiota between when the paired samples were collected.
How can Owlstone Medical help with your gut microbiome research?
As interdisciplinary specialists in breath, at Owlstone Medical, we designed the Breath Biopsy® Collection Station to allow reliable and reproducible breath collection, including efficient and portable ambient VOC exclusion, simultaneous collection of replicate samples, and easy collection of blanks.
The Collection Station is part of Breath Biopsy OMNI® our end-to-end optimized service for consistent breath analysis. Another aspect of OMNI is access to our VOC Atlas. Currently more than 200 rigorously identified VOCs are registered within the ATLAS, including gut microbiome-associated VOCs like sulfurous compounds, short-chain fatty acids (SCFAs) like acetate, butyrate, and propionate, and aromatic amino acid breakdown products.
You can find out more about working with us to investigate and monitor the gut microbiome in our webinar ‘’Non-invasive Functional Assessment of the Microbiome from Exhaled Breath’ or get in touch to talk to one of our in-house experts.