Distinguishing COPD from lung cancer in a large cohort study
Breath testing could help to differentiate help seekers with related symptoms
| Publication information: LuCID preliminary data
Disease Area: COPD, Lung cancer Application: Precsion Medicine Sample medium: Breath Products: ReCIVA® Breath Sampler, Breath Biopsy® Services Analysis approach: GC-MS Summary:
|
Chronic Obstructive Pulmonary Disease (COPD) refers to a group of diseases that cause airflow blockage and breathing-related problems. The Global Burden of Disease Study (2016) reported 251 million cases of COPD globally, contributing to around 5% of deaths (2015, 3.17 million)1. COPD is usually progressive, and exacerbations, which are typically related to viral or bacterial infections, are a major cause of lung function decline. Smoking is the most commonly encountered risk factor for COPD.
There has been an increasing call in recent years to explore precision medicine approaches to COPD, to help differentiate COPD from other respiratory conditions, monitor variation over time and help to predict and assess exacerbations.
VOCs and COPD
Breath VOCs have great potential to be used in the diagnosis of COPD. Patients being tested for COPD often have impaired lung function and so their ability to successfully complete spirometry tests is often limited. Since VOC analysis can be carried out using breath collected during regular tidal breathing, it is much easier to collect samples from patients. The ease of collecting breath samples with ReCIVA Breath Sampler has been assessed in a cohort of patients with acute breathlessness2.
Using Breath Biopsy to distinguish between patients with COPD and lung cancer
Evidence suggests that breath VOCs collected and analysed using Breath Biopsy can differentiate between COPD and other lung diseases. Figure 1 shows the performance of the platform in a population of 227 COPD patients and 269 lung cancer patients. Breath Biopsy was able to distinguish lung cancer patients from those with COPD with a sensitivity of 91% and a specificity of 64%. The area under the receiver operator curve equals 0.80 ± 0.03.
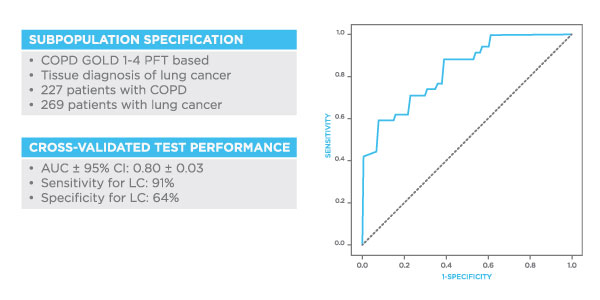
Figure 1. Results from Owlstone Medical’s Breath Biopsy platform showing the ability to use exhaled VOC analysis to differentiate between lung cancer and COPD. Sensitivity 91%, Specificity 64%, ROC 0.80.
Other Studies in COPD
A study of 28 COPD patients using GC-MS and electronic noses identified 19 VOCs correlated with the eosinophil cationic protein (ECP), a biomarker of eosinophil activity. Another four associated with myeloperoxidase (MPO) and neutrophilic marker3 (Figure 2). Analysis showed high sensitivity and specificity (AUC 1.00 for ECP, 0.96 for MPO) for mild COPD patients where inflammation prevails but not for moderate COPD patients which is dominated by airway remodelling. Another small study of 14 patients showed that VOCs on breath respond to treatments, with different patterns observed during treatment with beclomethasone/formoterol vs. fluticasone propionate/salmeterol4.
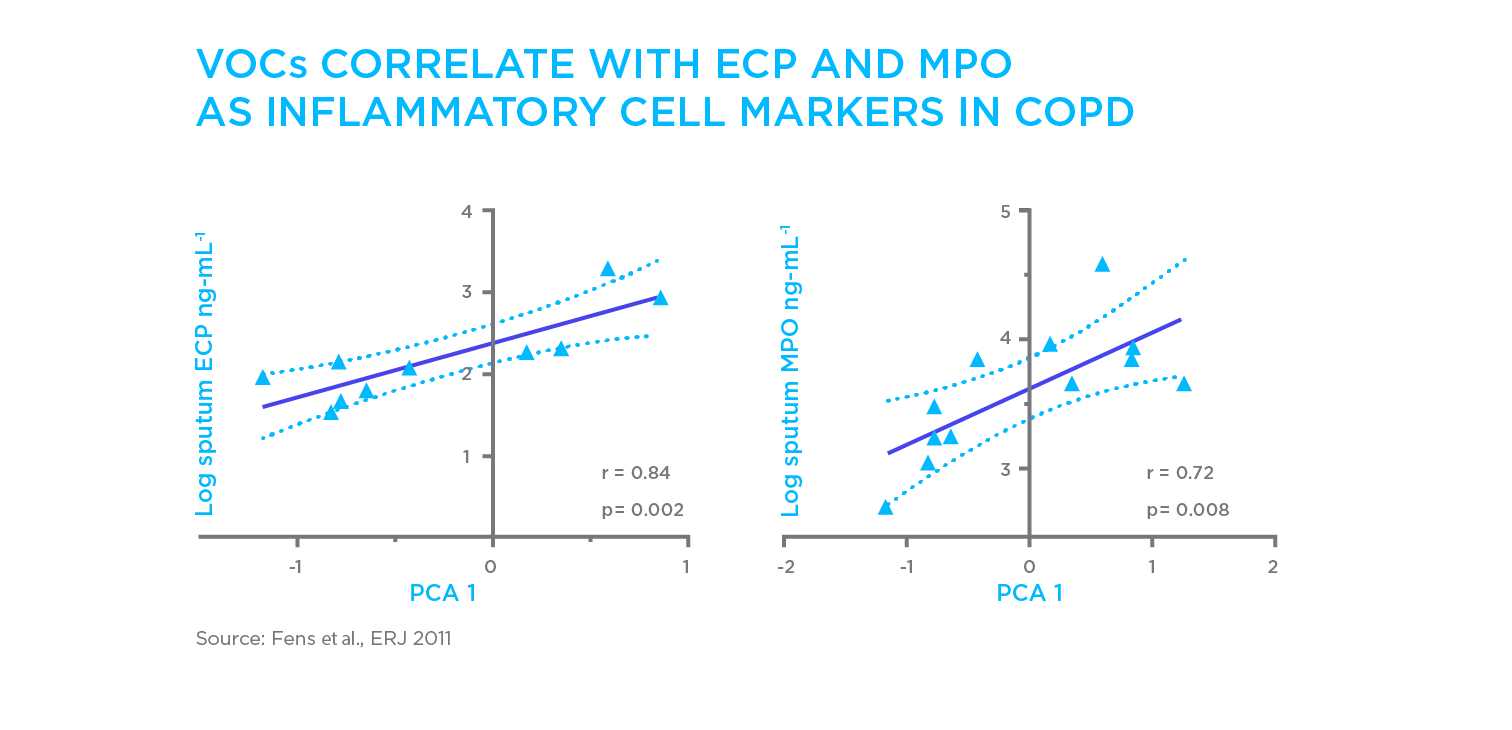
Figure 2. Identifying links between VOCs in breath and inflammatory biomarkers in different forms of COPD. ECP is a marker of activated eosinophils while MPO indicates neutrophil activity.
A systematic review5 of existing studies highlighted indole6, aromatic hydrocarbons, acetic acid, phenol7, hexanal, nonanal and decanal8, and 2-pentanone9 as VOCs with proposed associations with COPD. These VOCs have been used to create predictive models with between 70% and 92% correct classification rates.
References
- World Health Organization, COPD Fact Sheet 2017 https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
- Holden KA, Ibrahim W, Salman D, et al. (2020) Use of the ReCIVA device in breath sampling of patients with acute breathlessness: a feasibility study, ERJ Open Res. DOI: 10.1183/23120541.00119-2020
- Fens et al., Exhaled air molecular profiling in relation to inflammatory subtype and activity in COPD, Eur. Respir. J. (2011), 38(6):1301 – 1309. DOI: 10.1183/09031936.00032911
- Montuschi et al., Exhaled 8-isoprostane as an in vivo biomarker of lung oxidative stress in patients with COPD and healthy smokers. Am J Respir Crit Care Med. (2000) 162:1175–7. DOI: 10.1164/ajrccm.162.3.2001063
- Finamore et al., Breath analysis in respiratory diseases, state-of-the-art and future perspectives. J. Molecular Diagnositcs. (2018). 19 (10): 47-61. DOI: 10.1080/14737159.2019.1559052
- Sinues et al., Breath analysis in real time by mass spectrometry in chronic obstructive pulmonary disease. (2014), Respiration; 87: 301-310. DOI: 10.1159/000357785
- Phillips et al., Machine learning methods on exhaled volatile organic compounds for distinguishing COPD patients from healthy controls. (2012). J Breath Res; 6:036003. DOI: 10.1088/1752-7155/6/3/036003
- Basanta et al., Exhaled volatile organic compounds for phenotyping chronic obstructive pulmonary disease: a cross-sectional study. (2012). Respir Res. 13:72. DOI: 10.1186/1465-9921-13-72
- Allers et al., (2016). Measurement of exhaled volatile organic compounds from patients with chronic obstructive
pulmonary disease (COPD) using closed gas loop GC-IMS and GCAPCI-MS. J Breath Res. 10:026006. DOI: 10.1088/1752-7155/10/2/026004
Catch up on the presentations from the Breath Biopsy Conference 2024


